24 Weeks pregnant: Symptoms, baby development & tips
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways:
- Hormones, circulation, and fluid retention are all linked to a variety of skin-related symptoms like dryness, itchiness, hives, and rashes
- Your baby is working on producing important cells this week that help their lungs take in oxygen and expel carbon dioxide
- Most women will receive a glucose detection test between weeks 24 and 28 to screen for gestational diabetes
Welcome to week 24 of your pregnancy! In this week’s article, we will cover some changes you might experience in your appetite, skin, and muscles. We will also check in on your baby, who is working hard at gaining weight and developing their respiratory and neurological systems. We will also discuss what it means that your baby is viable this week and share important information about what preterm labor and delivery mean. Finally, we will wrap up with some tips for things you can do this week to support your health and prepare for your new baby.
Your body at week 24
Increased appetite
Between the disappearance of first-trimester nausea or morning sickness and the emergence of pregnancy cravings, you might notice you are hungrier than normal. During the second trimester, doctors advise adding around 340 calories daily [1]. Foods that are high in fiber, protein, healthy fats (like certain nuts and seeds, and avocado), and complex carbohydrates (like legumes, fruits, starchy vegetables, and wholegrain products) can all help you maintain a healthy pregnancy diet while keeping you feeling fuller, longer.
Rashes
Changes to hormones, fluid retention, and circulation can all affect your skin in different ways, including the development of itchiness, hives, or rashes linked to your pregnancy.
Itchiness caused by dry skin and stretch marks is common during pregnancy. Stretch marks (which we covered in the 17 weeks pregnant guide) are a type of scarring that is caused by the stretching of skin, like on your lower belly during pregnancy. Try to avoid scratching, as this can make itchiness from dry skin and stretch marks worse.
In rare cases, itchiness can be a sign of an uncommon but potentially serious liver condition known as intrahepatic cholestasis (ICP) of pregnancy [2]. ICP usually appears without a rash, but causes itchiness on the palms of the hands and soles of the feet that is sometimes worse at night. Other symptoms may include dark pee and pale poo [2].If you suspect you might have ICP, contact your healthcare provider immediately.
Hives are an allergic reaction that can result from exposure to certain foods, insect bites, medicine, chemicals, pollen, animal dander, or other substances. It is possible for you to develop hives due to exposure to things you might not have previously had a reaction to. Scientists believe that the body can become more sensitive to certain allergens during pregnancy [3]. It’s important to remember that hives can also be brought on by stress.
Rashes are typically separated into pre-existing or pregnancy-specific conditions. Psoriasis, one common pre-existing condition, usually improves during pregnancy, but can worsen postpartum [4]. Pregnancy-specific skin conditions, like atopic eruption of pregnancy (which includes prurigo and pregnancy eczema) and polymorphic eruption of pregnancy (also known as PUPPP), are less common [5]. Though uncomfortable, they are not known to cause any harm to the baby and are usually treated with pregnancy-safe anti-itch medications. For more on common and uncommon skin conditions, check out our 19 weeks pregnant guide.
Most minor rashes, including hives, typically go away on their own. Try to avoid scrubbing the affected area or using soap, as this can aggravate already sensitive skin. Keeping skin well-moisturized and avoiding long, hot showers and baths can also help prevent dryness and related itchiness. If you are suffering from a rash, or itchiness that does not resolve on its own, contact your healthcare team. There are over-the-counter and prescription medications available to treat skin conditions that are safe to take during pregnancy.
Carpal tunnel syndrome
Carpal tunnel syndrome (CTS) happens when the median nerve, which runs from your shoulder down into your hand, is compressed by the carpal ligament that sits in your lower palm. It is one of the most common hand injuries, more often experienced by women, and is usually caused by repetitive movements. Unfortunately, it is also commonly experienced in pregnancy, linked to hormone changes and fluid retention in the tissues that surround the median nerve in the wrist [6].
The main symptoms of CTS include tingling, aching, or numbness in the fingers and/or in the hand, usually in your dominant hand. CTS can also affect your ability to grip things or use fine motor skills. Symptoms usually resolve postpartum, when hormones balance out, but it's important to continue to be careful of your posture and not overstrain your wrist when feeding or holding your newborn.
Treating CTS during pregnancy can involve a combination of lifestyle changes and physical therapy. Eating a balanced diet that isn’t too high in salt and drinking enough water can help with fluid retention and swelling, while good posture can ensure you don’t place added strain on your already overworked muscular system. Wrist stretches and massage can both encourage fluid and blood circulation. Finally, elevation, rest, and cold compresses can all help with symptoms. In some cases, your doctor or physical therapist might recommend using a supportive hand or wrist splint, particularly at night, to help keep your hand in a neutral position while you sleep.
Your baby’s development at 24 weeks
Your baby’s brain, lungs, and taste buds are all growing and becoming more complex this week [7]. While the brain grows rapidly, the bronchi (main branches) of the lungs are developing special cells that help the lung’s alveoli take in oxygen and expel carbon dioxide. When premature babies have trouble breathing, it’s usually because these cells have not had enough time to develop.
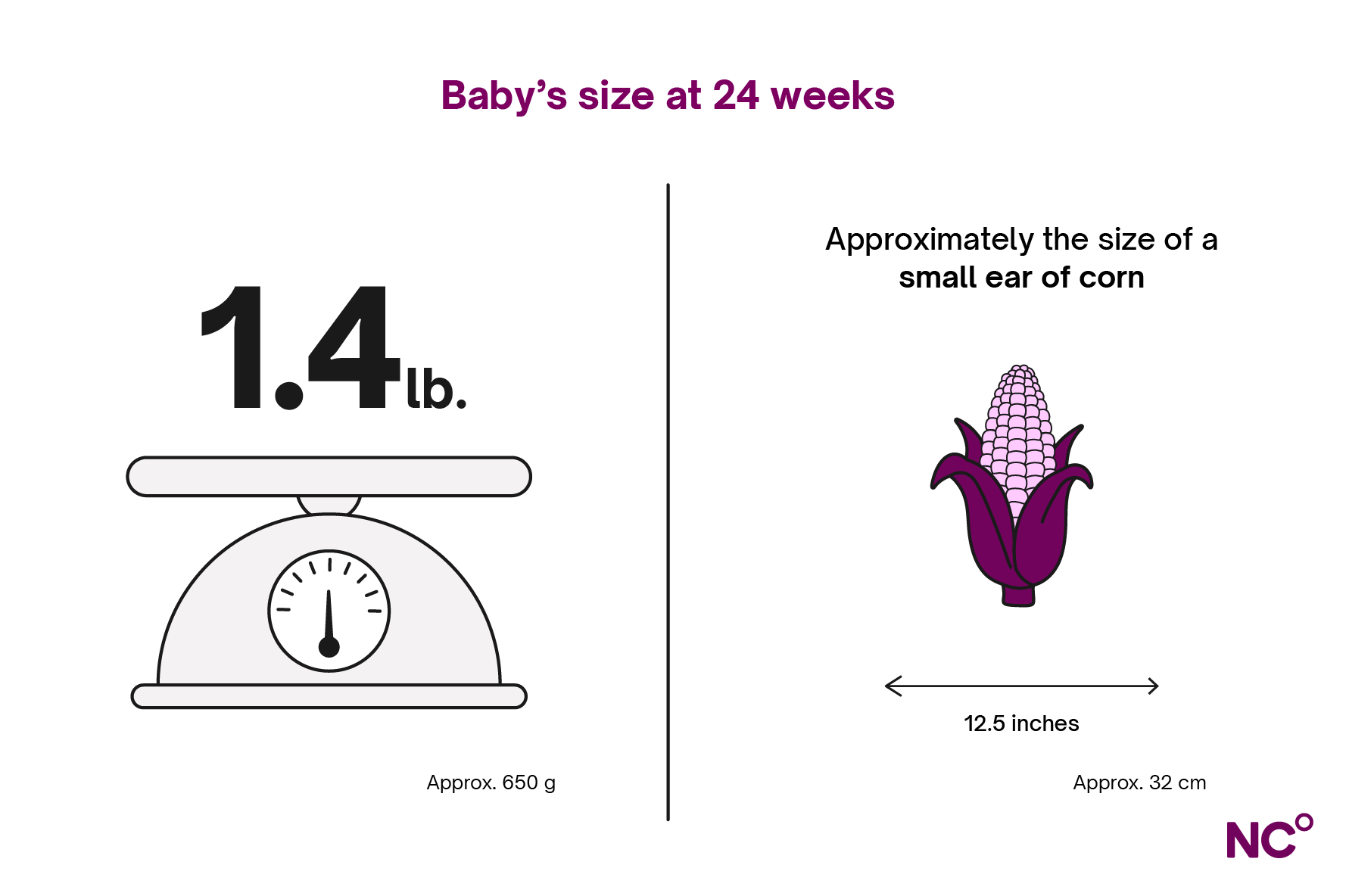
In week 24, your baby is around the size of a small ear of corn, measuring about 11.8 to 12.5 inches (30-32 centimeters) and weighing between 1.25 and 1.4 pounds (600-650 grams) [7].
Preterm labor and premature birth
Medically speaking, the term “viable” is used in two circumstances during your pregnancy. First, when examination shows that a pregnancy is expected to proceed normally, and second, from week 24, when your baby is considered to have a good chance of survival outside of the uterus, with proper medical care [8]. This might be scary to think about, and it's likely you have many weeks and months left in your pregnancy. However, it’s important to recognize the signs of preterm labor or serious medical issues so that you can seek immediate attention if needed.
Premature labor is labor that occurs before the 37th week of your pregnancy. Signs of premature labor include contractions or tightenings of your uterus, cramping, fluid leaking from your vagina (this could be your water breaking), and a backache that is unusual for you [9]. It is important to remember that preterm labor does not always lead to a preterm birth. Depending on your own health and the health of your baby, it is possible to receive treatment to delay birth, and in some cases, preterm labor can even stop on its own [10].
Tips in week 24
- Scheduling your glucose tolerance test: Most pregnant women are advised to receive a glucose tolerance test between weeks 24 and 28 to check for gestational diabetes. Gestational diabetes occurs when your body cannot produce enough insulin to help control your blood sugar levels. While gestational diabetes typically resolves once you give birth, having gestational diabetes increases the likelihood of having it again in future pregnancies and increases chance of developing type 2 diabetes in the future [11]. The goal of a screening test is to detect the condition so that it can be monitored. The test involves fasting for 8 to 10 hours, having a blood test, drinking a very sweet glucose drink, and then having another blood test to see how your body has processed the glucose.
- Thinking about contraception: While getting pregnant again might be the last thing on your mind, it’s important to remember that your body can begin ovulating around 4 to 6 weeks postpartum. It’s a good idea to start thinking about contraceptive options now. You can speak to your healthcare provider about the best options for you and use the opportunity to raise any questions about postpartum contraception. If you’re thinking about non-hormonal birth control, you can use Natural Cycles postpartum to support your recovery and help prevent pregnancy when ovulation returns.
- Start baby proofing: While it will be some time before your baby is moving around, those first months with your newborn will likely be full. Planning ahead and ensuring your home is safe will save time and stress later. Make sure smoke and carbon monoxide detectors are installed and working properly, cover outlets, and attach shelves, mirrors, and TVs securely to walls so they cannot fall. Baby locks on cabinets can also keep cleaning products and sharp kitchen utensils out of tiny hands.
- Go easy on hot showers and baths: While long, hot showers can be relaxing and soothing, they can also dry out your skin. If you find you are suffering from itchiness, unusually dry skin, or rashes, consider going easy on the heat or shortening your shower or bath time.
- Schedule your dental cleaning: Changes to your blood flow and body chemistry during pregnancy can contribute to increased prevalence of gum diseases like gingivitis and even tooth decay [12]. In addition to keeping up with daily flossing and brushing, don’t forget to schedule your routine cleanings and visits with a dentist or hygienist.
Did you enjoy reading this article?