Navigating PCOS: Dr. Krauss’ story
This PCOS Awareness Month, Dr. Kerry Krauss, board-certified OB-GYN and Senior Medical Advisor at Natural Cycles, walks us through her own experience of navigating PCOS. From fertility struggles to getting a diagnosis, read on to learn more about Dr. Krauss’ story and how using Natural Cycles can help you on your own reproductive health journey.
Periods, puberty & PCOS
I have personally struggled with polycystic ovary syndrome (PCOS) ever since I began having periods at age 11. Where my friends all had periods they could set their clocks to, mine were unpredictable and irregular from the start.
I also suffered from horrible cystic acne that I was unable to treat, even with the strictest skin care regimen, and that even persisted after trying extreme measures to control it, like daily antibiotic use and even Accutane (a type of retinoid medication).
In addition, despite being an athlete and runner and eating a well-balanced diet, I struggled with weight gain, which then led me to develop disordered eating behaviors.
Despite meeting several criteria for PCOS, neither I nor any of the doctors I saw connected the dots. My irregular periods? I could just go on the pill to fix that. Wouldn’t my acne eventually improve with age? And, maybe if I just decreased my calorie intake even further or exercised a little more, I could finally lose the 20lbs that would put me into the “healthy weight” category.
The fertility journey
It wasn’t until I was in medical school in my mid-20s that it first occurred to me that I might be struggling with PCOS. After marrying my husband in my second year, we decided that starting a family was very important to us, and since my mom had struggled with infertility, I knew that I would rather start trying to conceive sooner rather than later.
We had hoped to conceive by my third year, which would mean that our first child would be due during my fourth year of medical school, when the schedule allowed for several electives and easier clinical rotations. However, months went by, and even after timing intercourse around when I should have been ovulating, we failed to conceive after 9 months.
I began taking lots of ovulation tests, which is when I realized that in many of my cycles, ovulation occurred very late, if it even happened at all. We were lucky that we eventually conceived my daughter in the tenth month of trying, even though that now meant that I would deliver my first child right at the beginning of my residency training (probably the worst timing possible — it also meant very little maternity leave).
I had finally begun to suspect that I may have PCOS, given how inconsistent my cycles and ovulation were, but at that point, I was just happy to have conceived and didn’t give it much thought. I went back on hormonal birth control after I had my daughter, since it made my period more predictable, and as a new resident with a baby, it seemed like the easiest option.
However, with my second child, we again struggled to conceive. I was now five years older, and my cycles were even more irregular after coming off of hormonal birth control. It took me over a year to conceive my son, and then in my third trimester, I was devastated to discover that I had gestational diabetes.
This diagnosis led to a full-on emotional breakdown. I did not understand. I was doing everything right — I always counted calories, ate a high fiber and protein/veggie-rich diet, and exercised as much as my residency schedule allowed. Why was this happening to me? It seemed so unfair, but still (in what had become a pattern for me) I blamed myself for not having my body under “better control” — and now, this could lead to poorer outcomes for my unborn child.
I started monitoring my blood sugars and became increasingly frustrated that I could not seem to get them to where they needed to be, even when I would completely avoid any carbohydrates at all. I started insulin, and even then, I still struggled to maintain my sugar in a healthy range. I even failed to gain any weight for several weeks because I was essentially not eating any carbohydrates, and honestly, probably not enough calories.
This was the moment I realized that this was not normal — something else was going on that was beyond my ability to manage with just diet and exercise. And at this point, I had enough knowledge through my OB/GYN training to realize what no other doctor had told me up to that point — that my irregular cycles, terrible acne, inability to lose weight, difficulty conceiving, and now gestational diabetes, all fit with a diagnosis of PCOS.
Making sense of it all
But even the realization of my PCOS diagnosis did not offer me any profound solutions to my problems. After being a diabetic for three months, I really didn’t want to end up as a lifelong diabetic (which, as a gestational diabetic, I had up to a 70% chance of) [1]. But sadly, despite trying every diet on the market, my weight still ended up the same at the end, and even sometimes a bit higher, particularly after any very restrictive diet.
Even in my late 30s, I still had persistent acne, and my cycles continued to come anywhere from 25-45 days apart. Though I had hoped to avoid it, it was clear I was going to need some help from medication to help control my PCOS symptoms.
As an OB-GYN, I knew my medication options well. They included hormonal birth control to help regulate my cycles (and decrease my endometrial cancer risk), metformin to help with insulin resistance and weight loss, and spironolactone could decrease my androgen levels and help my acne.
I ended up trying all of these medications at various times (with varying degrees of success and/or side effects), but I was frustrated that there was no medication that could seemingly fix the “root cause” of my PCOS (spoiler alert: nobody, not even doctors, know what the root cause of PCOS is). I felt like I was in a war with my body, and even as an OB-GYN, I couldn’t seem to figure it out — which felt like both a personal and professional failure.
After years of being on and off of hormonal birth control, I decided to start tracking my cycles with Natural Cycles. I liked that I would not only be able to see how regular my cycles were, but know whether I was ovulating in each cycle.
Natural Cycles helped me realize that even in months when I had a normal cycle length, I often did not ovulate. This gave me crucial insight into how my PCOS was controlled (and also meant I could be at higher risk for uterine cancer)!. Coming up on my 40s, I knew my risks of diabetes, cancer, and obesity would only increase with time. Without a major change, things would only continue to get worse.
Managing my PCOS
When GLP-1 medications, like Ozempic, first came onto the market and took the world by storm, I was initially hesitant to try them. PCOS itself wasn’t a reason to take GLP-1 medication unless you were also obese or had diabetes. I didn’t even think it was an option for me (I was only “overweight”, and didn’t yet have type 2 diabetes) — or even if it was, I worried I would have to pay exorbitant prices if my insurance didn’t cover it (which many US insurances don’t).
Plus, I was already in the midst of trying other treatment options, such as going back on the pill (again), and enrolling in a program that allowed me to track my blood sugars with a continuous glucose monitor (CGM).
Knowing the correlation between my blood sugars and my exercise, sleep, and diet was a major breakthrough for me. As I suspected, even on days where my lifestyle factors were optimal, my blood sugars would swing wildly, and no amount of protein, fiber, or apple cider vinegar was bringing them down. It was clear to me that without some sort of outside intervention, I would likely end up diabetic in a few years.
It was this realization that led me to reconsider taking GLP-1 medication. I had heard from some OB-GYN colleagues interested in obesity medicine and PCOS that these medications had shown some early promise for PCOS patients (finally allowing them to lose weight, while also lowering androgen levels, regulating cycles, and improving insulin resistance). Natural Cycles’ own research has also shown GLP-1 medication might have a stabilizing effect on menstrual cycles. I decided to give it a try.
I have now been on a GLP-1 medication for close to a year. I am finally at a healthy BMI and have normal blood sugars again. Finding a treatment option that works for me has changed my life in ways I never thought it could, including dramatically improving my mental health. This may not necessarily be due to the treatment itself but might be due to finally being at peace with my diagnosis and no longer fighting against it (and my body).
I want to emphasize, though, that there is no one-size-fits-all treatment, and GLP-1 medications won’t be the best option for everyone with PCOS. It’s important to discuss all of your treatment options with a trusted healthcare professional and find what works for you.
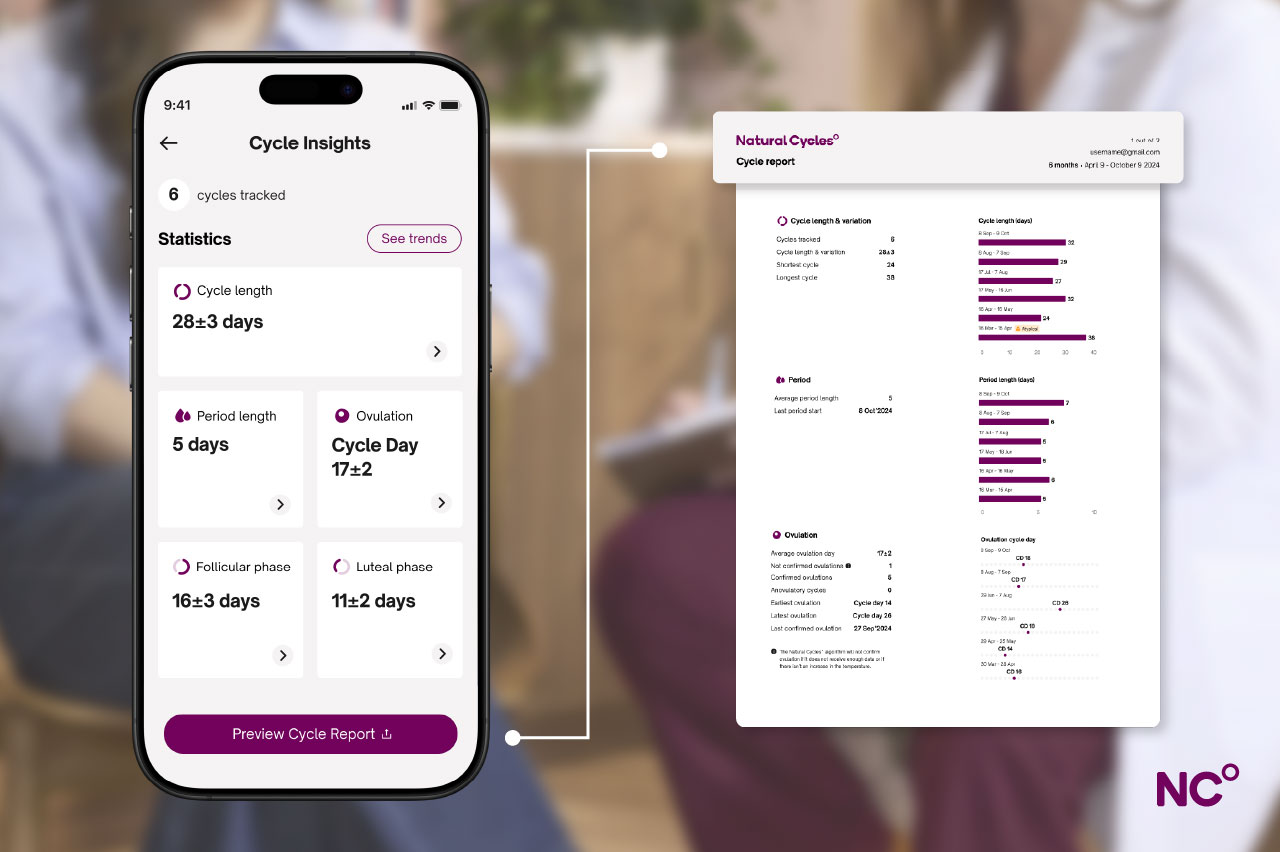
Natural Cycles can be a helpful tool on this journey to treatment too. The app makes cycle tracking easy and can even flag irregularities like skipped ovulation or a change in cycle length. You can easily share this with your doctor via the Cycle Report feature in the app — a feature I can’t recommend enough. You’ll find the link to download this detailed PDF under the Cycle Insights tab within the Natural Cycles app.
The key to treatment is diagnosis
Before women can get to the treatment of PCOS, they need a diagnosis. And even with a medical degree and most of my OB-GYN residency behind me, I was ultimately the one who put the pieces of my own diagnosis together. Many women with PCOS will see three different doctors and wait anywhere from two to five years to get a diagnosis [2].
I see so many patients who have struggled with irregular cycles, weight gain, acne, hair growth, infertility, and gestational diabetes or diabetes, and have never had anyone tell them their symptoms could be related to PCOS.
My heart breaks for these women, because knowing this diagnosis empowers them to get out of the cycle of shame of dealing with their symptoms in isolation and stop beating themselves up for things they can’t always control with diet and exercise alone (though these are still very important!).
It’s estimated that up to 50% of women with PCOS also have mood disorders such as depression, and I think that this could be partially due to difficulty getting an adequate diagnosis and treatment [3].
Know your body better with Natural Cycles
Everyone’s diagnostic and treatment journey looks different, but I truly believe there is no better way to empower yourself as a patient than to track your cycle. And, as a OB-GYN who both suffers from and treats PCOS, I love that Natural Cycles also gives insights into whether or not cycles are ovulatory, which makes a very big difference to PCOS patients.
Whether you choose to use Natural Cycles as a tool for diagnosis or as a means to track and manage symptoms beyond, keep in mind that the app can support you on your wider fertility journey too. The first FDA Cleared birth control app, Natural Cycles, is just as effective for those with irregular cycles. The certified medical device can also be used to plan pregnancy if and when you want to start a family. Finding your fertile days is such an important piece of the puzzle for those with irregular cycles.
If, after reading this article, you’d like to learn more about PCOS, check out the WHO’s fact sheet for more info. And know that if you suspect you have PCOS, you may unfortunately need to see more than one doctor to get a diagnosis. So always remember to advocate for yourself, come prepared with information, such as your Cycle Report. It’s important to know that PCOS is a treatable condition that doesn’t have to define you or how you live your life.
Thanks so much to Dr. Krauss for sharing her personal story with us. If you’d like to try Natural Cycles, you can use Dr. Krauss’ discount code via this link to access 20% off Natural Cycles and a free thermometer.
Did you enjoy reading this article?
