Perimenopause: Signs, symptoms & how to manage
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways
- Perimenopause is a natural phase of life leading up to menopause, the permanent stop of menstrual cycles, marking the end of our reproductive years
- Symptoms like period irregularities, night sweats, joint pain, and more can happen during perimenopause
- While everyone’s perimenopause experience is different, there are treatment options available for those who experience disruptive perimenopausal symptoms
On this page
- What is perimenopause?
- Can I get pregnant if I am perimenopausal?
- What is the typical age for perimenopause to start?
- How do you know you’re in perimenopause?
- Perimenopause tests
- Common signs and symptoms of perimenopause
- Treatments for perimenopause symptoms
- Signs perimenopause is ending
- Decode the menopausal shift with Natural Cycles
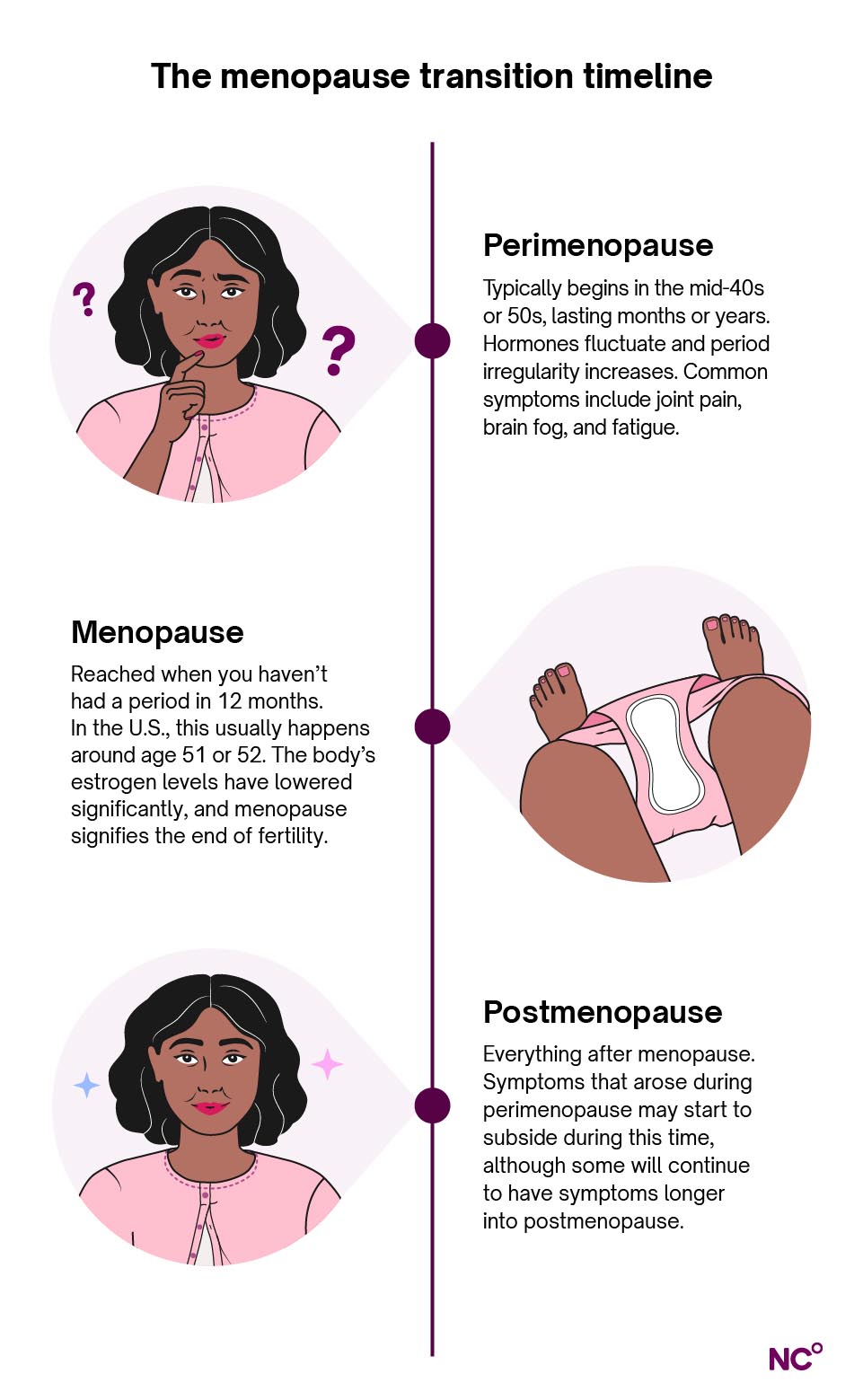
Perimenopause is a transitional time that leads to menopause, when menstruation stops completely, marking a new chapter in our lives. During perimenopause, we may notice periods becoming irregular, along with a host of other symptoms that are thought to be a result of the hormonal changes happening in our bodies [1].
In this guide to perimenopause, we’ll take a look at the signs and symptoms of perimenopause, commonly recommended treatments, and how tracking changes in your menstrual cycle can help you learn more about your body.
What is perimenopause?
Let’s start by defining perimenopause. It’s a natural phase of life for anyone who has a period. During this time, the body’s hormone levels fluctuate in preparation for the end of menstruation (menopause). It can come with symptoms like irregular periods, night sweats, joint pain, and more. While these symptoms can be disruptive, it’s important to know that everyone’s perimenopause journey is unique. You may experience all, some, or none of these symptoms in the lead up to menopause [1].
Perimenopause vs. menopause
A common point of confusion is the difference between perimenopause and menopause. The distinction between the two comes down to whether or not you still get your period — if you’re still menstruating, this means you’re still in perimenopause (even if it’s irregular).
Menopause is defined as the last menstrual bleed, this is diagnosed retrospectively after you haven't had a period for twelve months. Menopause marks the end of female fertility, your ovaries are no longer releasing egg cells, and your ovarian reserve (the amount of egg cells in your body that you’re born with) has naturally depleted. The period of time after menopause is reached is known as postmenopause [1, 2].
You may have heard the terms “perimenopause” and “menopause” used interchangeably in conversation, or “menopause” used to refer to the entire transitional phase — you may have even done this yourself! That’s okay, but we wanted to take this opportunity to clear up this often confusing terminology. Having access to more accurate terms to describe what happens in our bodies can empower us to identify irregularities, advocate for our bodies, and gain knowledge about our health.
What are the hormonal changes during perimenopause?
It’s thought that the wide hormonal fluctuations that occur during perimenopause may explain many of the symptoms associated with the transition, although more research is needed to confirm this link. For now, we know that there are four notable hormones at play during perimenopause — estrogen, progesterone, follicle stimulating hormone (FSH), and testosterone [2].
- Estrogen: Throughout perimenopause, estrogen levels can fluctuate. They’ll eventually end up lower than they were pre-menopause, but there are a lot of ups and downs in between. Estrogen levels affect both the urinary and reproductive systems, so if estrogen is declining at some point during perimenopause, this can lead to symptoms like vaginal dryness or more frequent UTIs.
- Progesterone: Similarly, progesterone levels will fluctuate during perimenopause. Progesterone levels can affect things like sleep, cycle length, and bleeding. Perimenopause symptoms will vary based on which of these hormones is dominant at any given time (estrogen or progesterone). More research is needed to understand these particular hormonal fluctuations.
- FSH: Follicle stimulating hormone might begin to rise earlier and more sharply during cycles in perimenopause. This is the body’s way of trying to stimulate every last egg cell. Levels of FSH remain high even after menopause.
- Testosterone: Testosterone levels tend to decline during perimenopause, which may lead to symptoms like low libido. [2]
Can I get pregnant if I am perimenopausal?
In short, the answer is yes. If you’re still getting periods, you’re probably still ovulating, meaning you can still conceive. However, ovulation becomes more unpredictable during perimenopause, in part due to these fluctuating hormones. With that in mind, it may be much more difficult for some people to get pregnant during these years. The risk of miscarriage and pregnancy complications also increases during perimenopause, but people do still have healthy pregnancies during this time [3].
If you’re experiencing perimenopausal symptoms and trying to get pregnant, it’s best to speak with your doctor for advice. If you don’t want to get pregnant during this time, it’s a good idea to keep using birth control until menopause [3].
Tracking ovulation and looking for patterns in your cycle may help you plan pregnancy or prevent it more effectively while going through perimenopause. Using tools like Natural Cycles, you can detect ovulation and pinpoint symptomatic patterns to understand your body better.
What is the typical age for perimenopause to start?
Most people begin to notice perimenopause symptoms in their 40s and 50s, usually between the ages of 45 and 55. However, it’s possible for perimenopause to start earlier in your 30s. In some cases, early menopause (not perimenopause) can occur due to medical procedures such as the surgical removal of both ovaries, chemotherapy, or radiation. This results in an immediate drop in estrogen levels and is known as induced menopause [1, 4].
[1, 5]
How long does perimenopause last?
As we mentioned earlier, the perimenopause experience (including symptoms and timeline) is highly variable. Your journey may look very different from someone else’s, so it can be difficult to predict your exact start of perimenopause. Once the transition starts, it can last anywhere from a few months to up to ten or more years. In the United States, women reach menopause around the age of 52 on average, marking the end of perimenopause [1].
How do you know you’re in perimenopause?
The exact start date of perimenopause may be difficult to predict. Signs of perimenopause can be subtle at first, and easy to overlook or attribute to other causes. Most people notice irregular periods as the first sign of perimenopause — this can mean longer or shorter cycles, longer or shorter periods, or heavier or lighter bleeding. According to some widely used medical frameworks, the perimenopause transition begins when there is at least a seven-day difference in cycle length from one cycle to the next [2]. But keep in mind that there are other causes of cycle variations, including conditions like PCOS.
With all of this in mind, it’s natural to feel a bit uncertain about what’s going on and when you’re in perimenopause. Factors like age and symptoms can be helpful when diagnosing perimenopause, but ultimately, tuning into your body and tracking changes over time can help you understand what phase you’re most likely in.
Perimenopause tests
While changes in our menstrual cycles are often the first sign of perimenopause, blood tests can also detect hormone levels that may indicate that you’re in this transition. Although some of these perimenopause tests detect high levels of FSH, this is actually not as reliable of a marker as a hormone called Anti-Müllerian Hormone (AMH).
Anti-Müllerian hormone (AMH) levels reflect your ovarian reserve and naturally decline with age. While AMH testing can help estimate how close you may be to menopause, sometimes within a window of a few years, it’s mostly used in research settings and not currently recommended as a standard tool to diagnose perimenopause. Research continues to improve the accuracy of these tests, and more sensitive versions are in development, but they are not yet available for routine clinical use [6].
For now, we primarily use menstrual cycle changes, symptoms, and timing to figure out where we are in our reproductive journeys. Making a habit of tracking your cycle length can make the process of identifying the start of perimenopause much easier. Logging dates and symptoms in the Natural Cycles app can give you deeper insight into what’s happening in your body and where you are in the menopause timeline.
Like mother, like daughterDid you know that the age your mom reached menopause can be a good indicator of your own journey, too? Research on mother-daughter pairs found that heredity (our genetic link to our mothers) played a substantial role in the timing of menopause [7]. |
Common signs and symptoms of perimenopause
Here is a list of notable symptoms associated with perimenopause to look out for as you’re assessing your own experience with this transition:
- Body odor changes
- Brain fog
- Breast soreness
- Cycle changes
- Fatigue
- Frequent urination
- Hair loss
- Heart palpitations
- Insomnia/trouble sleeping
- Joint pain
- Low libido
- Mood changes
- Night sweats/hot flashes
- Period changes
- Spotting
- Weight gain
- Vaginal dryness and painful sex [2, 8]
Remember that although these are common, your body is unique and you may not experience some (or any) of these symptoms. Their severity and duration may vary, as well.
Mood changes: What is perimenopause anxiety?
One of the perimenopause symptoms we want to highlight is mood changes, specifically perimenopause anxiety. It’s possible to experience challenges associated with your mood and emotions during perimenopause, and it’s important to seek the care and support you need to ease the burden. Women with a history of depression and/or anxiety are at risk for future depression, but in one study, researchers found that about 16% of perimenopausal women report new onset depression or anxiety during perimenopause [2]. Women are also twice as likely as men to be diagnosed with an anxiety disorder or depression.
Feeling anxious every now and then due to one-off stressors is a normal part of life, but if you’re consistently struggling with your mental health, it’s a good idea to seek help from therapy, along with exercising regularly and giving yourself opportunities to rest [9]. (We know, easier said than done.)
There’s no need to suffer in silence. Talk to your doctor or a friend you can trust, and if you experience very dark or suicidal thoughts, you can also reach out to the 988 suicide & crisis lifelife or access resources via their website.
Treatments for perimenopause symptoms
For individual advice and treatment options for managing perimenopause symptoms, we recommend speaking to your healthcare professional first and foremost. They can assess your unique situation and help chart the best course forward for you. They’ll likely recommend hormone therapy or lifestyle changes (or a combination of the two) to help you navigate this transition more comfortably.
We’ll go through the most commonly recommended treatments below, but first, we want to note that there’s no “cure” for perimenopause, as this condition will eventually affect anyone who gets a period. However, the symptoms associated with perimenopause can be severe and disruptive, and some may benefit from symptom treatment in an effort to ease the transition.
Hormone therapy
Hormone replacement therapy (also called HRT or menopausal hormone therapy, MHT) is one of the most widely recommended courses of treatment for severe perimenopause symptoms. It works by adding synthetic hormones that are at lower levels in your body during perimenopause and beyond [10].
If you’re looking for a jumping off point for a conversation with your doctor about HRT, here are a few common hormonal treatment options and what you should know about them:
|
Type of hormone therapy |
How it’s administered |
Who is this best for? |
Pros |
Cons |
|
Estrogen-only (topical or oral) |
Pill, patch, gel, spray |
Only recommended if you have had your womb removed during a hysterectomy. Otherwise, you’ll need to supplement with a progestin or use a combined HRT method to lower risk of endometrial cancer. |
Can address symptoms associated with decreased estrogen during perimenopause, such as vasomotor symptoms, genitourinary changes, joint pain, and mood and cognitive issues. |
You’ll need to supplement with progesterone/progestin if you have not had a hysterectomy. For oral HRT, there is a risk of forgetting to take pills, and pills can have a risk of blood clots. For topical HRT, it can take a few minutes or up to an hour before you can get dressed, shower, etc. Topical treatments can affect your surroundings (children, pets, etc.). |
|
Estrogen-only (vaginally inserted) |
Tablet, pessary, ring, gel, cream |
People whose symptoms are localized to the vaginal area and urinary system (such as dryness or pain during sex). |
Can ease vaginal dryness and pain during sex, as well as urinary symptoms like UTIs. Can also positively affect sex drive and ability to have an orgasm [23]. |
Has not been shown to help with hot flashes, mood swings, or sleeping problems. |
|
Progesterone/progestin- only* |
Pill, implant, IUD |
Recommended for those with irregular, long, or heavy periods, but who don’t have symptoms of declining estrogen [26]. |
Can help regulate the bleeding if you take progesterone 10-12 days per month. With the implant or IUD, you don’t usually bleed. |
Risk of forgetting to take the pill. Not as effective at treating vasomotor symptoms as oral or transdermal estrogen. Side effects include headaches, vaginal bleeding, and mood changes. With the implant or IUD, you may experience irregular spotting. |
|
Combined estrogen and progesterone/progestin |
Estrogen as pill, patch, gel or spray. Combined with progesterone as pills, capsule, or IUD. There are also fixed combinations (both hormones in the same pill or patch) and variants where you combine one estrogen and one progesterone medication. |
Most people who are experiencing moderate to severe perimenopause symptoms. |
Can address most symptoms associated with perimenopause. |
Risk of forgetting to take the pill or change the patch. Possible side effects like breast tenderness, spotting, bloating, mood changes, irregular bleeding. Estrogen pills come with an increased risk of blood clots, though the risk is still very small [24]. |
|
Testosterone** |
Gel |
Usually only recommended in late perimenopause or postmenopause and you have problems with sex drive/ability to orgasm that other forms of treatment (HRT, sex therapy, etc.) have not helped. |
Can increase libido and ability to orgasm. |
Possible side effects include acne, increased hair growth where the gel is applied, and weight gain, but these are not common at the doses used for perimenopause symptoms. |
*Progesterone is the hormone your body naturally produces (primarily in the ovaries). Progestins are synthetic compounds designed to mimic its effects. Together, they make up a family of chemicals called progestogens. In hormone therapy, you can be prescribed either progesterone (usually micronized or bioidentical) or a progestin (synthetic), depending on the goal of treatment and your doctor’s judgment.
**Testosterone is not currently licensed to treat symptoms associated with perimenopause, but speak to your doctor about whether a specialist can prescribe it if you’re interested in learning more. [11, 12, 13, 14, 15]
Hormone therapy is generally not suitable for those with:
- Current or past breast cancer. Systemic estrogen (e.g., pill) is contraindicated, but low-dose vaginal estrogen may be considered in select cases
- Vaginal bleeding with an unknown cause
- Current blood clots
- Serious liver or gall bladder disease
- Current or past history of angina, heart attack, or other heart problems [16]
If you have certain conditions, you should be careful with hormone therapy (speak to your doctor about treatment options and dosage):
- Migraine
- Diabetes with vascular effects
- History of blood clots
- Gall bladder disease
- History of endometrial cancer
- Lupus
- Dementia
- Asthma
- Epilepsy
- Porfyria
Non-hormonal medication
As an alternative to hormone therapy, there are several non-hormonal medications that can help address perimenopause symptoms. Antidepressants can help with sleep issues, mood changes, and hot flashes. An anti-seizure medication called gabapentin, along with a blood pressure medication called clonidine, can both reduce hot flashes and ease the sleep difficulties associated with perimenopause.
A more modern treatment is neurokinin receptor antagonists, which affect the temperature regulation center in the brain and are effective when treating hot flashes and sweating. Neurokinin receptor antagonists or SSRIs are good options for those who can’t use hormonal treatments due to other conditions. [17, 25, 27]. Note that treatment options for perimenopause symptoms may vary depending on your country/where you live.
What lifestyle changes can I make to manage perimenopause symptoms?
Many people also find that lifestyle changes can ease the severity of perimenopause symptoms as well. Here are some of the most common perimenopause lifestyle adjustments:
- Eat a nutritious diet: We’re told this our entire lives — eat your veggies! During perimenopause and beyond, it’s still important. Eating a diet rich in fruits, vegetables, and particularly calcium and protein, can help keep you healthy. The Mediterranean diet is a great guide for most people, but as long as you’re eating plenty of protein, fresh produce, whole grains, and omegas, you’re doing great.
- Take care of your body: A regular, gentle exercise routine can contribute to your overall health and support your body during this transition. It’s an individual journey to find what type of movement, intensity, and frequency work best for your body, but resistance training/lifting and recovery methods are generally recommended for this stage of life. Some people also find physical therapies like massage or acupuncture helpful.
- Create healthy sleeping habits: Make sure your sleep sanctuary is set up to your liking — a slightly chilly, dark room with minimal noise and comfortable bedding is recommended. Going to sleep and waking up around the same time each day can also make all the difference, and listen to your body’s signals to rest as you need to throughout the day.
- Maintain mindfulness: Deep breathing exercises and/or a meditation practice can boost your mental and emotional health day-to-day. Additionally, relaxation methods like certain forms of yoga or tai chi can integrate these practices and help to reduce stress. Undue stress can bring on hot flashes and other symptoms.
- Wear light clothing: You may be due for a new look! Try swapping out heavier clothing items for lighter layers and a more flowy wardrobe to keep you cool, relaxed, and comfortable. This is especially true for pajamas if you’re experiencing night sweats. It may help to have an extra pair on hand by your nightstand so that your sleep isn't interrupted by having to get up and change.
- Have cool drinks or a fan on hand: Having these resources available can help ease vasomotor symptoms like hot flashes and night sweats whenever they come up.
- Avoid common triggers: Spicy food, caffeine, hot drinks, smoking, and alcohol can all worsen the severity of perimenopause symptoms. Endocrine-disrupting chemicals (EDCs) are certain types of chemicals like phthalates and parabens that mimic hormones like estrogen and are found in many consumer goods. Although more research is needed in this area, EDCs have been linked to worsening perimenopause symptoms like hot flashes.
- Non-hormonal lubricants and creams: For vaginal dryness, there are non-hormonal options available without a prescription.
- Consider herbal supplements: Herbal supplements have been popular on the internet as a treatment for menopause. However, most of these have not been studied extensively, so they may not work the same way, or even be effective, for everyone. Always speak with your doctor before starting any new supplements.
- Get mental health support: It can help to speak with a therapist to deal with some of the mental and emotional struggles that come with perimenopause. Talking to others who are going through the same thing as you can also help ease the burden. Even nowadays, there can be so much stigma surrounding the topic of menopause that it stops us from talking about it, but sharing can be a helpful way to lighten the load.
[8, 14, 18, 19, 20, 21]
Signs perimenopause is ending
The end of perimenopause is menopause — that point on the timeline when it’s been 12 months since your last period started. After this point, postmenopause is the body’s new normal. This phase can come with lingering symptoms including hot flashes, sleep disturbances, and mood changes, along with genitourinary symptoms like frequent urination, vaginal dryness, and low libido. These symptoms usually subside in the coming years, but the hormone therapy options and/or lifestyle adjustments listed above can help in the meantime [22].
In postmenopause, there may also be an increased risk for certain health conditions like urinary tract infections (UTIs), heart disease, and osteoporosis due to decreased estrogen in the body. With that in mind, it’s important to maintain a healthy lifestyle and stay up-to-date with doctor visits and screenings throughout postmenopause to get the support you need in this new phase of life [5].
Decode the menopausal shift with Natural Cycles
Discover your perimenopausal stage, learn to navigate your symptoms and cycle changes, and unlock data-driven support with NC° Perimenopause, from Natural Cycles, the makers of the first FDA-cleared birth control app. Click "get started" to learn more about how Natural Cycles can support you throughout this journey.
NC° Perimenopause is here to support you with wellness insights and information. It’s not a diagnosis — we always recommend consulting with your own doctor for medical advice.
Did you enjoy reading this article?
