Signs perimenopause is ending
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways:
- Perimenopause refers to the years before menopause, when erratically fluctuating hormones can cause symptoms such as irregular periods, brain fog, and anxiety
- The start of perimenopause can happen as early as your 30s, but on average, most will start this transition phase between the ages of 45 and 55
- There is no set length of time that perimenopause will last, but there are signs that you are progressing through the late stage of perimenopause, such as an extended time between periods
- Everyone’s perimenopause experience is unique to them and shouldn’t be compared to that of others — tracking your cycle and symptoms can help you learn more about your body as you progress through this stage of life
Perimenopause is a natural transition phase as we approach menopause. But many of us can experience uncomfortable symptoms, and often find ourselves wondering: when does perimenopause end? In this article, we will look at when perimenopause starts, how long it lasts, and the signs that perimenopause is ending.
When does perimenopause start?
Let’s first remind ourselves what we mean by perimenopause and menopause. Menopause is the natural end of your fertile years, defined as the moment of your last period and diagnosed retrospectively after you have not had another period for 12 months [1]. Perimenopause is the period of time before you reach menopause, when hormones fluctuate erratically and can cause symptoms such as irregular periods, brain fog, and anxiety. After menopause, you transition to the postmenopause phase.
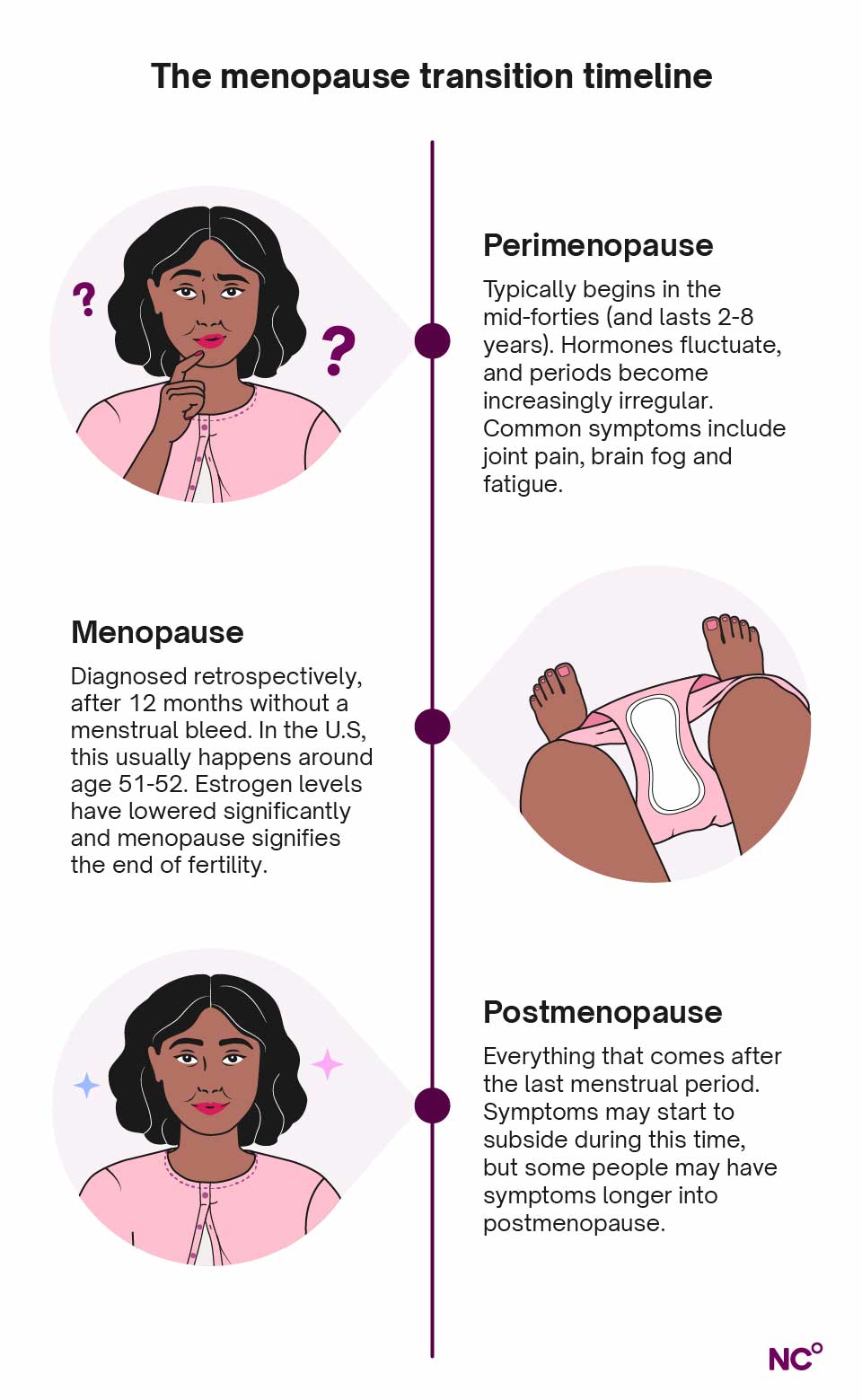
Perimenopause usually starts between the ages of 45 and 55, and the average age to reach menopause — and the end of perimenopause — is 52 [2]. However, this can vary drastically from person to person. Reaching menopause before the age of 45 is classed as early menopause [3], and premature menopause happens when you reach menopause before the age of 40. These earlier transitions may be caused by genetics or by medical procedures such as chemotherapy, radiation, or the surgical removal of the ovaries [4, 5]. It is also possible to experience late menopause, after the age of 55.
How long does perimenopause last?
Everyone’s perimenopause experience is highly individual, and your journey may differ from other people’s experiences. Whilst the median length of transition sits at four years [6], some may experience symptoms for longer than 10 years, and others for only a few months.
Many factors, including your environment, lifestyle choices, and genetics, shape your personal experience. For example, those with a higher body mass index are more likely to start perimenopause at a later age, with no impact on duration [6]. On the other hand, smoking can lead to earlier perimenopause, more severe symptoms, and shorter duration of menopausal transition. Race also plays a role. African-American women were found to experience longer menopausal transitions than white women.
Transitioning to menopause
It can help to visualize perimenopause in two stages: early and late. Early-stage perimenopause is when your hormones first start to fluctuate more erratically than usual, and symptoms begin to show. Often, the initial symptoms of perimenopause can be challenging to pinpoint, especially if you are taking combined hormonal birth control. This is because hormonal birth control often inhibits ovulation [7], and instead of a natural period, you experience a withdrawal bleed.
The most noticeable sign of starting perimenopause is irregular or missed periods [6]. Research in the field suggests early-stage perimenopause begins when there is a 7-day difference or more in the length of consecutive menstrual cycles. However, many conditions can cause irregular periods and changes in the menstrual cycle, such as stress, drastic weight changes, PCOS, endometriosis, or sexually transmitted infections [8]. If you notice irregular periods and suspect perimenopause, make sure you speak to your doctor to rule out other potential causes.
When you experience at least 60 days between periods, you are considered to be in late-stage perimenopause, which usually lasts for one to three years [6]. Hormones continue to fluctuate, but estrogen stays more consistently low. This drop in hormones can intensify perimenopause symptoms.
Signs perimenopause is ending
As you progress through late-stage perimenopause, the time between periods often increases, and periods can become even more irregular [6]. Bleeding can vary in heaviness, but you can still have both anovulatory and ovulatory cycles. Anxiety and depression are also common symptoms that can intensify as you progress through perimenopause. One study found that mid-life women are more likely to experience depression during perimenopause and postmenopause than premenopause, even when accounting for external factors [9]. Other symptoms that may intensify include hot flashes, night sweats, weight gain, and fatigue.
Remember, the symptoms you have and their severity will be unique to you and differ from what others experience. Always speak to your healthcare provider if you experience changes in your menstrual cycle or severe symptoms, and know that you are not alone if you need medical support. One study showed that nearly 90% of women sought medical attention for menopausal symptoms [10].
Are there tests to determine if you’re in menopause?
Yes, there are tests that detect hormone levels and can help determine if you are in perimenopause. Tests have traditionally concentrated on the follicle-stimulating hormone (FSH). But we now know that testing for Anti-Müllerian hormone (AMH) is a more accurate marker of your ovarian reserves, and, as such, can more reliably indicate how long to go until the final menstrual period. AMH testing is primarily used in research, and while there is growing promise for its use as a clinical test, it is not yet recommended for diagnosing menopause in a general healthcare setting [11].
At present, the most important indicator for perimenopause is the appearance of particular menstrual changes and symptoms. By tracking menstrual cycle length and characteristics with Natural Cycles, it is easier to notice irregular periods, changes in your menstrual cycle, and new or changing symptoms. You can also download your Cycle Report to take to your doctor.
Tips to manage perimenopause symptoms
Hormonal and non-hormonal treatments
There are specific treatments available to help ease perimenopause symptoms, and some can improve certain aspects of health during this transition, such as bone health. Hormone therapy, also known as hormone replacement therapy or HRT, is the provision of synthetic estrogen and progesterone (or sometimes progesterone only) to top up the hormones we naturally produce less of during perimenopause [16]. It is used to reduce the severity of perimenopause symptoms and can help protect from bone loss that occurs during perimenopause [12]. If you are avoiding pregnancy and using contraception, hormonal contraception such as the combined pill can double as a symptom reliever, too.
Hormonal treatments and hormonal birth control are not suitable for everyone, and there are non-hormonal alternatives that tackle specific symptoms. Antidepressants can help with depression, anxiety, and sleep issues. If you struggle with hot flashes, anti-seizure medication called gabapentin can reduce severity, while also helping with sleep, as can clonidine, a blood pressure medicine. Neurokinin receptor antagonists are a modern treatment for temperature regulation that can ease hot flashes [17].
Using treatments for perimenopause symptoms, whether hormone therapy, hormonal contraceptives, or non-hormone alternatives, is entirely optional and should always be discussed with your doctor before starting treatment. The treatment options available to you may also vary depending on your location.
Lifestyle changes
Whether or not you choose to use specific treatments for perimenopause, there are also several lifestyle changes you can make to reduce the severity of your symptoms, support overall health, and improve your comfort during this transition.
- Avoid hormone disruptors: Prolonged exposure to endocrine-disrupting chemicals (EDCs) could contribute to earlier menopause and increased severity of symptoms. While some EDC exposure is environmental and out of our hands, quitting smoking and reducing alcohol consumption are two lifestyle changes that can lower your EDC exposure and therefore contribute to less intense perimenopause symptoms, better cardiovascular health, and a lower risk of osteoporosis [12, 13].
- Eat a nutritious diet: Most of us know that nutrition is vital for health at any stage of life. But did you know that certain nutrients can help support bone health in perimenopause? Ensuring you get enough calcium, vitamin D, and protein in your diet can help promote healthy bones and muscles [14].
- Get regular exercise: Regular movement is beneficial at all stages of life for circulation, sleep regulation, and cardiovascular health. During perimenopause and the first years of postmenopause, strength training is particularly important for supporting bone health and maintaining muscle mass [15]. If strength training is new to you, you can start with gentle resistance band or dumbbell exercises at home.
- Wear light clothing: You might not be able to control the onset of hot flushes, but wearing loose, light fabrics can help you cool down and feel more comfortable throughout the day. Similarly, if you experience night sweats, lightweight pyjamas can help reduce your temperature and improve your sleep.
- Optimize your sleep environment: Speaking of sleep, a consistent nighttime routine and a comfortable sleeping environment can make a big difference in tackling sleep problems and feeling good the following day. Try to go to bed at the same time each night and reduce exposure to blue light from phones, TVs, and laptops in the hours before sleep. Keep your bedroom cool and minimize light as much as possible. Eye masks and earplugs can be handy for blocking unwanted light and sound.
- Talk to someone: If you are struggling with emotional changes, depression, or anxiety, it can be helpful to talk about it. You could confide in a friend or partner, join a support group, or speak to your doctor about professional support. Having a safe space to share your experiences can go a long way in improving your mental health and reminding you that you are not alone.
When to speak to a doctor
You should speak to your doctor if you experience symptoms of perimenopause or notice anything out of the ordinary with your cycle, such as unexplained bleeding or pain. Irregular periods and many of the other perimenopause symptoms can also be symptoms of other infections or conditions. If you think you are going through perimenopause, you should also speak to your doctor before starting any hormonal treatments, to make sure you choose the best option for your needs.
Get to know your cycle with NC°
When it comes to perimenopause, there is no “normal”, and everyone’s experience is unique. Natural Cycles is here to help you learn about your body and cycle throughout this stage of life. NC° Perimenopause is designed to support you with tracking symptoms and spotting patterns, with the option of recording HRT use, if you choose to use it. Along the way, the app will offer expert guidance and insights to help you better understand the changes you are experiencing.
Did you enjoy reading this article?
