How long do sperm live: Sperm life cycle & survival rate
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways
- Sperm can live for up to five days inside the female reproductive system under the right conditions, and survive indefinitely if they’re frozen, but they will quickly die on dry surfaces or in water
- Each ejaculation contains millions of sperm cells, but it only takes one sperm to reach the egg to get pregnant
- Sperm is produced continuously in the testicles, and the sperm life cycle takes around two and a half months from start to finish
Have you ever wondered how long sperm can live after ejaculation? Then you’ve come to the right place. Sperm can stay alive for up to five days in the female reproductive system, but sperm survival varies greatly depending on the environment they end up in. In this article, we’ll dive into the details about how long sperm can live under different circumstances, how sperm survival is connected to our fertility, what the sperm life cycle looks like, and how to improve sperm quality.
This article is also available in Spanish
How long do sperm live?
Most of us have probably heard some variation of a rumor or urban legend about someone who got pregnant from sitting on a toilet seat or swimming in a hot tub. So, can that actually happen? Long story short: no.
Sperm production takes around two and a half months from start to finish (no pun intended). But how long sperm can survive after ejaculation depends on where it ends up — it can range from minutes on a dry surface to decades in cryogenic storage. Inside the female reproductive system, sperm can live for five days under the right conditions [1].
Sperm are sensitive, and to survive and remain able to fertilize an egg cell, they need their environment to have the right temperature, pH level, and moisture [2, 3]. So, let’s take a look at how long sperm can survive under some normal and extreme conditions:
- Inside the female body: Amazingly, sperm can live inside the female reproductive system for up to five days — but only when the conditions are just right. Before ovulation, our bodies can promote sperm survival by producing a type of cervical mucus that makes it easier for them to get to the fallopian tubes, where fertilization takes place. [1]. This type of cervical mucus is often called fertile or egg white cervical mucus. Without it, sperm can only survive for a very short period of time.
- On dry surfaces: Semen needs to liquify (essentially become more fluid) for sperm to be able to travel to fertilize an egg [4]. Sperm won’t live long outside the body if they land on dry surfaces like bed sheets or skin. When exposed to the air, they will quickly dry out and die.
- In water: Not only will sperm disperse in water and become separated from the fluids that protect them, but they also require the right pH level to stay viable. Plus, any soap or chemicals in the water will kill off sperm pretty quickly. If you have unprotected sex in water, there is a risk of pregnancy, but you can’t get pregnant just from being in the water of a swimming pool or hot tub where sperm is present.
- Cryogenic storage: It’s possible to freeze sperm to use at a later time in a process called cryopreservation, for example, before undergoing certain medical treatments or if you're doing IVF. When stored at a cryobank, sperm samples are kept at a consistent freezing temperature of -196°C, where they can survive indefinitely [5]. Many sperm banks allow you to store sperm for several decades, but make sure you check with the specific facility if you’re considering this option.
To sum up, while sperm can live for a few days in the female reproductive system, they won’t survive very long outside the body unless they’re stored in very specific conditions, like a cryobank.
How much sperm does it take to get pregnant?
Even though each ejaculation contains millions of sperm, only one sperm will eventually fertilize the egg cell. That means that any time you have unprotected vaginal sex — and you’re in the fertile window of your menstrual cycle — you can technically become pregnant.
How much sperm is in an ejaculation?
A normal sperm count — the concentration of sperm cells in your semen — is anywhere between 20 and 150 million sperm per milliliter of semen, and one ejaculation is usually around 1.5 to 5 milliliters of semen (roughly between half and a whole teaspoon) [6]. Doing the math, that’s a lot of sperm cells in just one ejaculation.
Even though the words sperm and semen (or even cum) are often used interchangeably, they aren’t exactly the same thing. The individual sperm are the male reproductive cells, meaning the cells that contain the genetic information that results in a fetus if it’s combined with an egg cell. Semen refers to the ejaculate and is made up of seminal fluid, which contains the sperm and helps to protect and transport them [7].
Does pre-cum contain sperm?
It can, but it doesn’t always. Pre-cum, or pre-ejaculation fluid, is a clear fluid that comes out of the penis during arousal. The purpose of pre-cum is to make the urethra less acidic (urine is acidic, and if you remember, sperm is sensitive to pH levels), and it also helps with lubrication [8].
Pre-cum isn’t produced in the same place as semen and doesn’t contain sperm in itself, but it can mix with semen or pick up sperm that’s left in the urethra. There have been some small studies looking into how common it is for pre-cum to contain sperm, with results varying between roughly 17-40% of samples [9, 10]. The most important thing to know is that you can get pregnant from pre-cum, which is one of the reasons why the pull out method (withdrawal) isn’t very effective when it comes to preventing pregnancy.
How does sperm survival affect the fertile window?
You can’t get pregnant every day of your menstrual cycle. In fact, you’re only fertile for six days in any given cycle — this is called the fertile window, and it’s intimately connected to sperm survival. That’s because the length of the fertile window is determined by how long the sperm cells and the egg cell can live.
The fertile window consists of the five days leading up to ovulation and the ovulation day itself [11]. Sperm cells can stay alive for up to five days inside the female reproductive system under the right conditions (that’s the five days before ovulation), and the egg can live for up to 24 hours once it’s released on ovulation day.
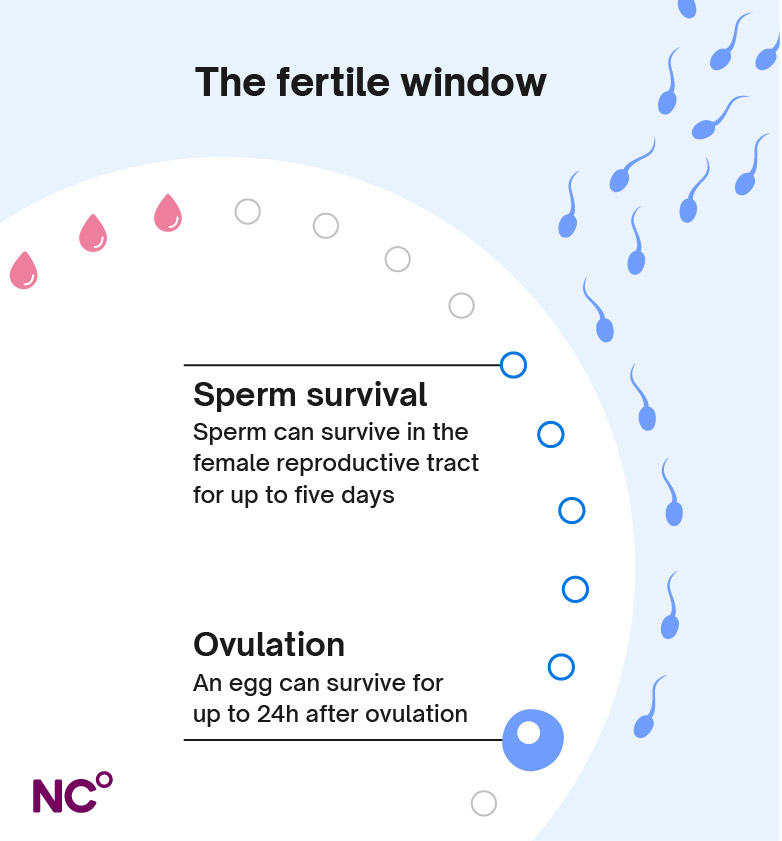
Cervical mucus also plays an important role in the fertile window when it comes to sperm survival. Our cervical mucus will change depending on where we are in our cycle. Just before and during ovulation, it becomes clear, wet, and slippery, creating a sperm-friendly environment that can help protect the sperm and allow it to stay alive longer. Even with these optimal conditions, only a small number of sperm will survive the swim and make it to the fallopian tubes to meet the egg [1]. At other times in the cycle when cervical mucus doesn’t have these qualities, sperm can only survive for a very short time.
How understanding the fertile window can help you get pregnant
If you’re trying to get pregnant, finding your fertile days is key, as it’s only during these days that sex can lead to pregnancy. Even though the whole fertile window is six days long, the likelihood of conception is higher during the days closest to ovulation [12]. Having sex right before ovulation happens means that the sperm have time to get to the fallopian tube, where they can wait for the egg to be released.
When using Natural Cycles to plan a pregnancy, the algorithm behind the app will calculate which days in your cycle you’re most likely to be fertile so that you can time sex accordingly and maximize your chances.
Sperm survival and preventing pregnancy
Sperm survival is equally relevant if you don’t want to get pregnant. Different birth control methods have different ways of ensuring that sperm can’t reach an egg, which is an effective way of preventing pregnancy. Barrier methods like condoms stop sperm from getting into the vagina, while other methods, like the birth control pill, stop ovulation from happening [13].
Many options, both hormonal birth control methods like the pill, IUD, or implant, and the non-hormonal copper IUD, also work by affecting sperm’s ability to survive in the female body. By creating an inhospitable environment for sperm, they cause sperm to die off quickly so they don’t have a chance to reach the egg [13, 14].
But another way of preventing pregnancy is by avoiding unprotected sex during the fertile window altogether — the key is just knowing when those days are. NC° Birth Control lets you do just that. By analyzing your body temperature and menstrual cycle characteristics, the algorithm behind the app detects your ovulation and estimates your fertile days in each cycle, so that you know when you need to use protection during sex (or abstain) and when you don’t. The NC° app automatically takes sperm survival into account when flagging possible fertile days, by assuming a fertile window of six days and adding an individual buffer to account for changes in ovulation day from one cycle to the next.
What is the life cycle of a sperm?
In contrast to female egg cells (we’re born with all our eggs), sperm production happens continuously in a process called spermatogenesis. In this process, many sperm are produced each day — a normal sperm count is anywhere between 20 to 150 million sperm per milliliter of semen [6].
Even though sperm can only survive for a relatively short time after ejaculation, the sperm life cycle is actually quite long, around 70 days in total [15]. Very simplified, the process looks like this:
- Immature sperm cells will divide multiple times within the testicles, and eventually form into the tadpole-like cells (with a head and tail) we recognize as sperm.
- Once they have their form, sperm move from the testicles into the epididymis (which is essentially a long tube), where they spend around two weeks maturing even further, acquiring the ability to move and fertilize an egg.
- During ejaculation, sperm move into the vas deferens (sperm duct) and are then ejected through the urethra. If ejaculation doesn’t happen, the sperm are reabsorbed by the body.
How does health impact sperm quality?
If you’re trying to get pregnant, sperm production can affect the chances of conception. It’s important to have a healthy sperm count, meaning that you produce enough sperm, as well as produce sperm of good quality. This means that the sperm have good motility (they’re able to swim well) and that there aren’t a lot of sperm with damaged DNA. Good quality sperm have a better chance of surviving and fertilizing the egg cell.
Men’s fertility isn’t as tied to age as it is for women, and men can continue to produce sperm throughout their lifetime. However, with increasing age, the quality of the sperm and the amount of sperm produced (also known as sperm count) may degrade [16]. For sperm to be made, the testicles and the hormone-producing glands that help to trigger sperm production need to function normally, and while we can’t remove the effects of age, the best way to promote sperm quality is to lead a healthy lifestyle. You should also speak with your doctor if you have any concerns about your sperm.
How to improve sperm quality or sperm count
A healthy lifestyle can help promote good sperm quality. If you’re thinking of lifestyle changes as part of planning for a pregnancy, one thing to keep in mind is that it takes roughly two and a half months for new sperm to form. That means it will also take roughly the same amount of time for lifestyle changes to take effect on sperm quality.
Here are some tips that you or your partner can try to promote sperm production and quality:
- Eat a healthy diet: A balanced diet that includes plenty of fiber, vegetables, and fruit can help make sure sperm production is optimal [16]
- Maintain a healthy weight: Weight can impact our fertility. When it comes to sperm production, obesity has been linked with both a lower sperm count and sperm quality, and some research also shows that being underweight can result in a lower sperm count [16, 17].
- Minimize stress: High stress levels have been linked with lower sperm count and quality, and it’s thought that this is due to stress affecting the hormones that control sperm production. However, it’s also important to note that fertility issues are stressful on their own, and it’s not entirely clear what causes what. All in all, reducing stress whenever possible can have a positive effect on fertility as well as our overall well-being [16].
- Exercise regularly: Including exercise in your routine can also help boost fertility. Studies have found that moderate exercise is good for promoting sperm health, and men who are physically active tend to have better sperm quality [16].
- Eat enough zinc: Zinc is an important micronutrient for male fertility due to its antioxidant and testosterone-promoting qualities, while a zinc deficit has been linked with lower sperm production [18]. Eating foods such as seeds, nuts, and wholegrains can help you get enough zinc. If you’re thinking of adding supplements to your diet, make sure to speak with your doctor first.
- Keep testicles cool: There’s a reason why the testicles are located outside the body — sperm need to stay a little bit cooler than our core body temperature. Indeed, heat has been shown to have a negative impact on sperm production, so trying to keep the testicles cool by wearing loose-fitting underwear and avoiding sitting down for too long can be a good idea [16]. Some very small studies have also suggested that avoiding hot tubs and saunas may be beneficial, but more research is needed in this area [19, 20].
- Quit smoking and recreational drug use: Smoking and use of drugs like marijuana, cocaine, opioids, and anabolic steroids have also been linked with reduced sperm count or quality, so it’s best to avoid them altogether [16].
- Limit alcohol: You can still likely have a drink now and then, but limiting your alcohol intake can also have a positive effect on fertility. While it’s not entirely clear at exactly what doses alcohol impacts sperm production, a high alcohol intake has been shown to lower sperm count and quality [16].
Leading a healthy lifestyle is a great way to promote fertility, but we can’t control everything ourselves. As always, when it comes to our health, it’s important to get the right help when we need it. If you’re concerned about sperm quality or having trouble conceiving, it’s a good idea to speak to a healthcare professional to get the help you need.
When to speak to a doctor
Trouble conceiving can happen due to a number of reasons, and the most common cause for men is that there is some issue with their sperm. A doctor can do a semen analysis to evaluate sperm count and sperm motility, as well as test hormone levels that can affect sperm production [21].
It’s normal that it can take a while to get pregnant, and if the female partner is under 35 and neither of you has any known fertility issues, you’re usually recommended to try for a year before seeking help. If the female partner is older than 35, you can seek support sooner, usually after trying for six months [21].
It’s just as common for men to have fertility problems as women. In one-third of cases where couples struggle to conceive, the issue lies with sperm quality or another issue pertaining to male fertility. One-third is due to a problem with female fertility, and one-third is due to a combination of both or unknown causes [22].
Prevent or plan a pregnancy with Natural Cycles
The fact that sperm can live for up to five days in the female body is a key aspect of our fertility, both when it comes to birth control and pregnancy planning. By analyzing your body temperature and unique cycle patterns, and by taking sperm survival into account, the NC° algorithm finds your fertile window (those six days in the cycle when you can get pregnant). When you know your fertile days, you can choose to either use a condom or abstain from sex if you’re using NC° Birth Control, or plan intercourse on the days you have the best chance of conceiving when using NC° Plan Pregnancy. Natural Cycles caters to your unique fertility journey. Why not find out if it could work for you today?
Did you enjoy reading this article?