Withdrawal bleeding: Overview, causes & symptoms
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways:
-
The bleeding that happens when you're on hormonal contraception is actually not a period but withdrawal bleeding
- Not all people experience withdrawal bleeding while on hormonal contraception, and the bleeding might be lighter and shorter in duration than a regular period
- While the chances of getting pregnant during withdrawal bleeding are low, no birth control method is 100% effective
This article is also available in Spanish.
The bleeding you experience while on different types of hormonal birth control, such as the contraceptive pill, is not a menstrual bleed. It is a type of bleeding known as withdrawal bleeding.
Many brands of combined birth control pills available on the market offer 28-day packs, with 21 pills containing hormones and seven hormone-free placebo pills (or sugar pills) that can be taken in the last week of the cycle. During that fourth week, people will experience bleeding. Did you know that this bleed isn’t the same as your period? This is known as withdrawal bleeding.
How long does withdrawal bleeding last?
The duration of withdrawal bleeding can vary from person to person, but most often, it lasts between four and seven days. However, if you have prolonged withdrawal bleeding or heavy bleeding that's starting to interfere with your everyday life, it's a good idea to speak to your doctor and perhaps consider switching birth control methods.
The origin of the withdrawal bleed
Despite what you might think, withdrawal bleeding doesn't have any major medical health benefits or risks. Many women on hormonal birth control prefer to experience a withdrawal bleed because they find it reassuring that the birth control is working and that they aren't pregnant (although it's worth noting that spotting can happen in early pregnancy; this is known as implantation bleeding).
When the birth control pill was first made available back in the 1960s, it was decided that a break inbetween pill packets should be used in order to mimic the menstrual cycle. The reasons for that were more cultural than medical.
These days, it is becoming more common for individuals to take birth control pills without taking sugar pills or a break between pill packets. However, the accepted normality of the withdrawal bleed — and the misconceptions around it — is a stark reminder of the ways in which reproductive rights have been constrained and influenced by more factors than simply our own well-being.
Withdrawal bleeding vs. period
So, what's the difference between withdrawal bleeding vs. period? Before we compare the two, let's first define menstruation. Each new menstrual cycle begins with a period. This bleeding is triggered by a drop in progesterone levels and increased levels of prostaglandins that cause the lining of the uterus to shed if the implantation of a fertilized egg cell hasn't happened by the end of the menstrual cycle.
Withdrawal bleeding is different from a period because many hormonal birth control medications stop ovulation from happening. This means when we're on certain types of birth control, we technically don't experience a regular menstrual cycle and period.
Another thing that makes withdrawal bleeding a bit different is the amount of blood involved. Bleeding on birth control is often lighter and shorter than a regular period because the contraceptive hormones stop the uterine lining from fully developing before it sheds.
Withdrawal bleeding vs. breakthrough bleeding
As mentioned above, withdrawal bleeding happens during the last week of your four-week hormonal birth control course. You might experience random spotting throughout the month. It's called breakthrough bleeding.
This type of breakthrough bleeding can happen for various reasons [1], and it rarely signals a health problem. In fact, breakthrough bleeding is fairly common when using many types of hormonal birth control, including the combined pill, the mini-pill, and hormonal IUDs, especially in the first few months of starting a new medication.
If you experience frequent breakthrough bleeding, and it's interfering with your daily life, you might want to speak with your doctor about options, such as changing the type of birth control method you're on.
Reasons for bleeding on birth control
Withdrawal bleeding happens when there is a change in hormone levels. When you take a scheduled break on the fourth week from taking hormonal birth control, you experience a change in hormones, which causes the bleeding.
You might also experience a withdrawal bleed if you switch to a new type of hormonal birth control, and it's common to experience a one-off withdrawal bleed when you take emergency birth control, like Plan B, which contains a higher dose of hormones.
Can you have withdrawal bleeding after stopping birth control?
You can experience a form of withdrawal bleeding when you stop any hormonal birth control (and might also experience it when you transition to a new method). It's completely normal, so while it can be inconvenient, it’s usually not a cause for concern.
If you are switching from hormonal birth control to a non-hormonal method, be aware that it can take a little while for your cycles to become regular again and for ovulation to resume. This is very individual and will depend on a number of things, such as how long you have been using hormonal birth control, what the method was, and, of course, your own health and the regularity of your cycle.
Can withdrawal bleeding be avoided completely when taking birth control?
Some people choose to skip the breaks and avoid the withdrawal bleeding completely. They start a new cycle of the pill, ring, or patch again immediately after 21 days.
People choose to use these birth control methods continually to treat symptoms of conditions like endometriosis and to help relieve headaches, bloating, tiredness, and other menstrual symptoms and pains. It can also be used as a method to delay bleeding if you have a vacation planned or a big event coming up. It's generally safe to do this [2], but it's always best to consult your doctor before you change the way you use your prescribed method of birth control.
What types of birth control have built-in withdrawal bleeding?
Not all types of hormonal birth control cause withdrawal bleeding. Let's review the most popular birth control methods that incorporate scheduled breaks during which withdrawal bleeding happens:
The combined pill
A combined pill uses the combination of the hormones estrogen and progesterone to stop ovulation and prevent pregnancy from happening. The combined birth control pill comes in different doses of hormones and packets of 21, 28, or 90 days, with a break usually prescribed between these doses.[3] During that break, you take inactive pills or placebo pills, and this is when the withdrawal bleeding happens.
The vaginal ring (NuvaRing)
A vaginal ring is a small, flexible ring containing a dose of hormones. It's inserted inside the vagina for a period of 21 days. After 21 days or three weeks, the ring is removed for a week, during which withdrawal bleeding happens. After the break, a new ring is inserted for another cycle.
The hormonal patch
A hormonal patch contains estrogen and progestin (the synthetic form of the hormone progesterone). It's worn on the chest, stomach, buttocks, or upper arms. A new patch is worn every week for three weeks. During the fourth week, you take a break from wearing a patch, and this is when the withdrawal bleeding happens. After the fourth week, you apply a new patch and repeat the cycle.
Alternative hormonal methods
Not all hormonal birth control options come with scheduled bleeding. Other methods are used continuously. However, it’s worth noting that you may experience breakthrough bleeding or spotting on these methods, particularly in the first few months of switching to this type of birth control. These methods include:
Intrauterine devices (IUDs)
There are two different types of IUDs available: hormonal IUDs that contain progestin and last between three to eight years (like Mirena) and copper IUDs that are hormone-free and are effective for up to ten years (like Paragard).
When you're using a copper IUD, you'll have your regular periods because it's a hormone-free birth control method. They might be different (lighter or heavier), especially in the first few months after the IUD is inserted.
If you're using a hormonal IUD, then you might have light bleeding, or you might not. It'll often depend on the hormonal dose in your IUD.
Implant
A birth control implant (like Nexplanon) is a small, thin rod about the size of a matchstick that's inserted under the skin on your upper arm. It contains the hormone progestin, which is released from the implant into your body and stops pregnancy by preventing ovulation and making the cervical mucus thicker, which limits sperm mobility. The implant can be effective for up to five years.
While using the implant, you might experience heavier bleeding (especially in the first few months), long-term spotting, or you might stop bleeding altogether.
Contraceptive injection
There are several types of birth control shot, including, Depo-Provera. This is a hormonal injection you can get every three months (guidelines will vary with different brands of shot). Many individuals choose this form of birth control because of its convenience. The shot contains the hormone progestin, which stops you from getting pregnant by preventing ovulation. It also makes cervical mucus thicker, which makes it harder for the sperm to move through the female reproductive tract.
When it comes to bleeding while on the shot, almost half of the people lose their periods completely. [4] It's completely normal, nothing to worry about. During the first year of being on the shot, you might experience heavier bleeding, spotting, or you might stop bleeding completely.
Mini pill
A mini pill is a type of oral contraceptive that contains only the synthetic hormone progestin. It prevents pregnancy by stopping ovulation and making the cervical mucus lighter, which impacts sperm mobility.
A mini pill is different from a combined pill because there are no scheduled breaks between pill packs. You take a pill a day, and each pill contains hormones. So, you might stop bleeding altogether while you're on the mini pill, or you might have spotting and, in some cases, irregular breakthrough bleeding that might be heavier or lighter than your regular period.
Sex during withdrawal bleeding
You can definitely have sex during withdrawal bleeding. It's a bit like having sex while you're on your period (although you may find it’s less messy due to a lighter bleed). Bleeding is an effect of hormonal birth control and nothing to be concerned about. Whether or not you choose to have sex while bleeding is an individual choice.
The chances of getting pregnant are extremely low when you’re using the pill, patch, or ring if you've taken your hormonal contraception as prescribed. However, since no birth control method is 100% effective, if you are sexually active, there is always a chance of pregnancy.
If you've been sexually active and know that you might have missed a day of your hormonal birth control, or you've discontinued hormonal birth control and haven't experienced a withdrawal bleed within two to four weeks, then it's a good idea to take a pregnancy test.
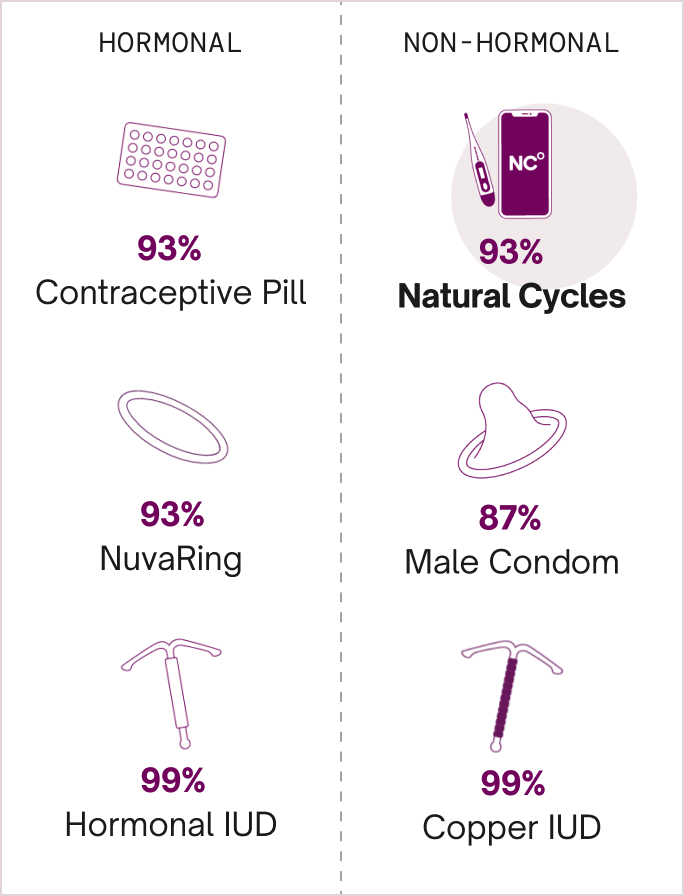
The pill, patch, and ring are all 93% effective with typical use and are more than 99% effective at preventing pregnancy with perfect use.
Discover hormone-free birth control
So, to sum things up, the bleeding you experience while on hormonal birth control or right after you've stopped using it is not your period but withdrawal bleeding. Periods can only happen if you're ovulating, and hormonal birth control prevents that from happening.
Thinking about moving away from hormonal birth control? Switching to a hormone-free method can help you understand the pattern of your cycle and is a great way to get to know your body better. Natural Cycles works by finding and predicting your ovulation using your body temperature paired with a smart algorithm, forming the world's first birth control app.
To date, over 3 million women have registered to use Natural Cycles, each embarking on their own hormone-free journey. If you're thinking about going hormone-free, why not find out if Natural Cycles could work for you?
Did you enjoy reading this article?