History of birth control: Timeline & when was it legalized?
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways:
- The history of birth control is paved with methods that range from the strange, like putting fruit in your vagina or jumping backwards, to the dangerous, like drinking toxic copper water
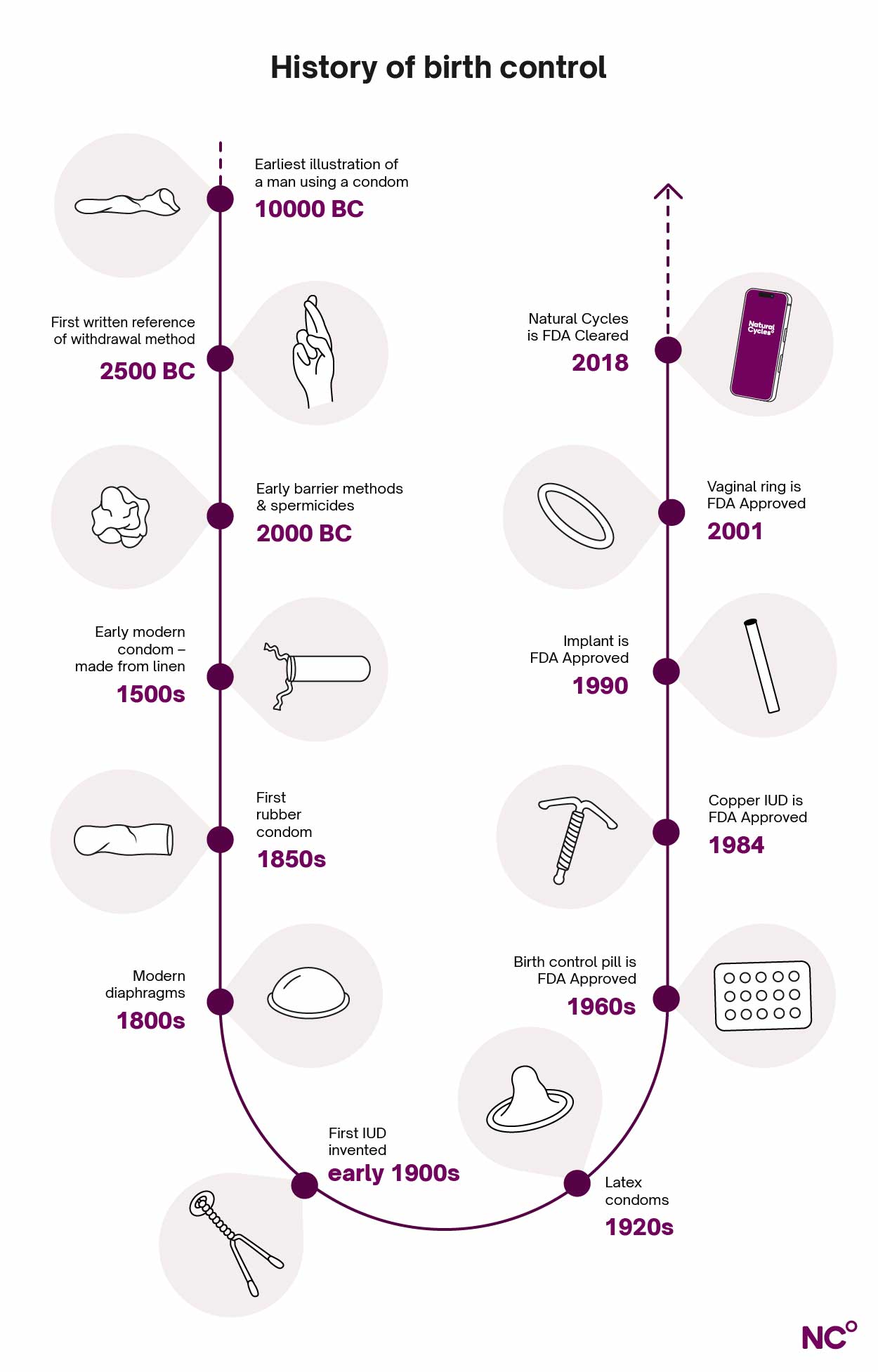
- Some methods are really old: the first mention of the withdrawal method dates back 2,500 years, while early versions of barrier methods and spermicides were already being used around 2000 BC
- The last 200 years have brought many innovations in the history of birth control, from the rubber condom in the 1860s, the first IUD in 1909, the development and legalization of the birth control pill in the 1960s and ‘70s, to the invention of Natural Cycles in 2013
On this page
- What did we even do before birth control?
- Questionable advice from the history of birth control
- Barrier methods have been around for a long time
- The history of fertility awareness methods
- History of the birth control pill
- Other short- and medium-acting methods
- Long-acting reversible contraception (LARC)
- Changing the game: Natural Cycles
- Understand your options with Natural Cycles
The history of birth control is a long one, filled with weird misunderstandings, amazing discoveries, revolutionary inventions, and animal poop (yes, poop). In this article, we’ll travel back in time and walk you through some of the birth control methods that brought us to where we are today. From ancient Egypt to modern-day Sweden, we’ll dive into the history of barrier methods, hormonal contraceptives, and more.
What did we even do before birth control?
As long as humans have walked the earth, we’ve had sex. But many birth control methods as we know them today — as pills, implants, shots, and so on — only became available pretty recently, so what did they do back in the day to avoid getting pregnant? Before we jump into the (at times, quite bizarre) history of birth control, let’s travel back even further.
It’s easy to think that people just got pregnant left and right before we had birth control. However, while there aren’t any written sources from back when we were hunters and gatherers, researchers are fairly certain that women tended to have children at least a few years apart. This happened naturally since babies were breastfed for several years, which naturally suppressed fertility [1].
Implications of birth control for women’s reproductive freedom
We can’t talk about the history of birth control without also touching on the implications it’s had for women’s reproductive freedom. The ability to control if and when you have kids without having to abstain from sex has played a huge role in women’s autonomy and in the women’s rights movement. Birth control being legalized and made available meant that more women were able to complete higher education and join the workforce [2].
During the sexual revolution of the 60s and 70s, when perceptions around sex became more open, the birth control pill and other contraceptive methods also meant that women were able to enjoy their sexuality without fear of becoming pregnant [3]. So, without further ado, let’s jump into the history of birth control.
The pull out method is really, really, really old
The pull out method, or withdrawal method, is probably one of the oldest ways of preventing pregnancy. It’s done by removing the penis from the vagina before ejaculation. One of the first mentions of it dates back to the story of Onan in the Torah, and this reference is more than 2,500 years old [3]. There are also records of the pull out method being used in ancient China and India [3]. However, the method itself likely predates these written records. While we’ll never know who came up with it (no pun intended) or when it was first used, we’re certain that it’s been around for a long time.
Today, the pull out method is still widely used [4]. While it does have some natural advantages — it’s free, and easily available — it’s simply not that effective (80% with typical use) [5]. Keep in mind that timing withdrawal can be tricky and even if it’s timed properly, you can get pregnant from pre-ejaculate if it gets into the vagina. That’s right, you can get pregnant from pre-cum!
Questionable advice from the history of birth control
Let’s fast-forward a bit in history because we need to address some… odd… methods.
Drink something toxic
The ancient Greeks gave us many great things, like democracy, theater and the Olympics, but their advice on the birth control front wasn’t always golden, to say the least.
Different harmful concoctions have been used throughout the history of birth control. Around 500 BC, Hippocrates, who is often referred to as the father of Western medicine, suggested that women drink copper salt water to avoid pregnancy [6]. For obvious reasons, this wasn’t effective (plus, copper is toxic to ingest), so we’re glad this advice didn’t live on.
Advice that might make your partner ask questions…
You’d think giving the ancient Greeks a few hundred years would provide some extra time to think, but it didn’t improve things. During the 2nd century, gynecologist Soranus gave us not one, but three unhelpful tips! He suggested women should:
- Hold their breath during sex (making us wonder about Soranus’ stamina)
- Sneeze after sex so the semen comes out (bless you?)
- Jump backwards seven times after sex (forget about after sex cuddles) [6]
We’d love to tell you that this was where the weirdness stopped. But alas.
You put the lemon where?
In the 1700s, the infamous lothario Casanova reportedly asked his lovers to use halved lemons as a kind of cervical cap to prevent pregnancy, and he even takes credit for this “invention” in his autobiography [3]. In truth, he didn’t come up with the idea that fruit juice might kill off sperm (inserting cotton or wool soaked in fruit juice was done at least since 2000 BC) [7]. But maybe he was the first one to skip the middle step and just put the entire lemon half in there. We’re not sure.
We don’t have any numbers on the birth control effectiveness of these citrus-based contraceptives, but they’re definitely not doctor-recommended today. While it’s possible the natural acidity of a lemon might act as a kind of spermicide and kill off straggling sperm (yes, there are studies on this [8]), the whole thing sounds a bit too… zingy for our taste.
Interestingly, there are some methods today, for example the vaginal gel Phexxi, that build on knowledge that acidity can affect the environment in the vagina and make it harder for sperm to swim. Phexxi isn't suitable for those with a history of UTIs and is 86% effective with typical use [9].
Barrier methods have been around for a long time
Barrier methods are a type of contraception that physically stops the sperm from reaching the egg cell. These types of methods have been around for millennia, and looking back at those first versions, we’re glad that there have been some improvements over the years.
Old-school methods that weren’t for the fainthearted
So, where might Casanova have gotten his inspiration? The earliest use of methods that resemble diaphragms, cervical caps, or spermicides dates back to at least 2000 BC, and the use of these early versions continued well into the Middle Ages [7, 10]. However, they certainly weren’t made of the same materials we’re used to today. Had you lived during that time, you may have found yourself putting some of the following into your vagina:
- Cotton or wool soaked in oils, fruit juice, or herbs
- Honey
- Grass
- Seaweed
- Crocodile or elephant dung
- Wine
- Rock salt
- Sponges (a version of which is still in use today!) [3, 7, 10]
Essentially, this is a list of things you don’t want to put in your vagina, but we might file this under “make do with what you’ve got”. After all, both barrier methods to stop sperm and spermicides to kill off sperm are still used today, albeit in different formats.
Modern barrier methods take shape
In the 1800s, we start to see the emergence of a diaphragm that looks more like what’s on the market today. The first custom-made rubber cervical caps were developed in Germany in the 1830s, and improvements continued during the rest of the century [3].
After learning about diaphragms during a trip to Holland in 1915, Margaret Sanger, founder of Planned Parenthood, played a big role in making diaphragms available and legal in the US. Because it was illegal to distribute contraception in the US during the beginning of the 20th century (laws at the time prohibited any medication or objects that could be used to prevent conception [11]), she had to smuggle diaphragms into the country. She ended up getting caught, but later won a legal case allowing them to be imported. By the 1940s, diaphragms were the most popular contraceptive method in the US, although it was later outcompeted by other methods, like the birth control pill [3].
Condoms weren’t always a walk in the park either
The condom is one of the most widely used birth control methods today, and it’s actually one of the oldest too. But there was a long road from the first condoms to the modern ones we now know. Let’s take a look at some highlights in the history of the condom:
- Condom cave paintings: The earliest record of a condom is from a cave painting in France, which depicts a man using a condom during sex. This painting is estimated to be 12,000–15,000 years old [3]. We don’t know exactly how condoms were used that far back, but we still think it’s pretty cool!
- Protection against serpents and scorpions: The first known written mention of a condom comes from the story of King Minos of Crete, who was thought to have lived in 3000 BC. It actually references a female condom — according to legend, King Minos’ sperm contained “serpents and scorpions” and to protect herself, his wife put the bladder of a goat into her vagina [12]. It’s hardly hard facts, but the story does show a cultural awareness of barrier methods and how they are used.
- Condoms made from animal intestines: The ancient Egyptians were early adopters of the condom. Records from 1300 BC show that they used sheaths to cover the penis [10], and early condoms were also used in Ancient Rome, Greece, China, Japan, and New Guinea. These early condoms were often made of animal intestines, animal bladders, or silk paper [12].
- …or linen: Some early condoms were fashioned out of linen. In fact, one of the earliest mentions of condoms in the modern sense is from the 1500s, when scientist Gabriele Falloppio conducted experiments showing that condoms in the form of linen sheaths protected against syphilis [12]. Hurray for protection against STIs, but does anyone else feel like linen condoms must have been a bit scratchy for everyone involved?
- Finally, rubber! It wasn’t until 1844 when Charles Goodyear patented vulcanized rubber that the condom we know today really started to take shape. By 1860, condoms were pretty widely available [12].
Today, condoms are made from latex, polyurethane (a type of soft plastic), or polyisoprene (synthetic rubber). While contemporary condoms might look (and feel!) radically different, the way we use them hasn’t changed — today, many people still rely on condoms both to prevent pregnancy and to protect against STIs. All hail the humble condom!
A note on male birth control optionsAside from the condom, there aren’t that many options when it comes to birth control for men. Other methods include using the withdrawal method (which isn’t very effective) or permanent options like vasectomy. There have been studies trying to develop hormonal birth control options for men, but none have yet made it to the market [13]. |
The history of fertility awareness methods
Fertility awareness methods (FAMs) — methods that rely on understanding when you’re fertile during the menstrual cycle — have also been around for a while.
FAMs as we know them today started cropping up during the 1900s, but already in the 17th and 18th centuries, African and Native American women understood that cervical mucus was linked to fertility and used this knowledge to prevent or plan pregnancy. Western medicine only caught onto this in the 1960s, when the Billing Method (or cervical mucus method) was introduced [3].
Using the menstrual cycle to predict fertility
It wasn’t until the 1920s that scientists discovered when ovulation happens in the menstrual cycle. From that initial discovery that ovulation, on average, happens 14 days before the next period bleed starts, the first calendar method was developed [14].
Of course, now we know more. In a study on more than 600,000 cycles from Natural Cycles users, we busted the myth that the average cycle is 28 days and also found that the average luteal phase is actually 12 days long. At the same time, the timing of ovulation varies from person to person, emphasizing the importance of solutions tailored to the individual, like the NC° app [15].
Turning up the heat with the temperature method
The fact that ovulation doesn’t always happen on the same day also played a role in how other FAMs developed, since this highlighted the need for more information than just counting cycle days.
Another important discovery in the field of fertility was that basal body temperature (BBT) is linked to ovulation. In the 1930s, Dr. Rudolf Vollman and his wife, Emmi, found that a rise in BBT is a reliable way to confirm that ovulation has happened [14]. This discovery paved the way for the temperature method, also known as the BBT method, where the user measures their BBT throughout the menstrual cycle to find their ovulation and fertile days.
FAMs continued to develop during the later part of the 1900s, and the sympto-thermal method is one such example — this combines BBT tracking with charting other symptoms during the menstrual cycle, like cervical mucus or luteinizing hormone (LH).
Fertility awareness in the smartphone era
Among the latest developments in the FAM world were smartphones, which allow users to track their symptoms in different types of apps. But advances didn’t stop there: in 2018, Natural Cycles became the first birth control app to be FDA Cleared as a method of contraception, marking a new era of digital birth control.
History of the birth control pill
The launch of the birth control pill is considered a landmark moment in the history of birth control and reproductive health more widely. Even though the first birth control pill was FDA approved in 1960, the research that laid the groundwork for it started decades earlier. A key discovery was that the female sex hormones that govern the menstrual cycle, estrogen and progesterone, could be used to inhibit ovulation in animals [16].
This research started in the 1920s and continued during the following decades, but it wasn’t until the 50s that it started being implemented for birth control. Margaret Sanger, founder of Planned Parenthood, along with her friend Katharine Dexter McCormick, funded research which eventually led to the development of the first ever birth control pill, which contained a combination of synthetic progesterone and estrogen [3].
When did the birth control pill become legalized?
Despite the FDA approval in 1960, it took a bit longer before the pill became widely available in the United States. At the time, the use of contraceptives was still restricted in the US through laws that banned the use of any object or medication designed to prevent pregnancy.
In 1965, Planned Parenthood won a case that rolled back the ban on married couples using contraception [3]. Legal battles over the birth control pill continued for several years, and it wasn’t until 1972 that the Supreme Court legalized all forms of birth control for everyone in the US — meaning that unmarried women were also able to access the pill [1, 2].
The safety concern
Even after the birth control pill entered the market, there were concerns about its safety. The first-generation birth control pills contained much higher doses of hormones than we now know are required, which meant that there was a higher risk of side effects, such as blood clots [16].
Research into the birth control pill continued, and this resulted in many improvements. The birth control pill as we know it today is very different from the first pills in its composition. The doses of the hormones in the pills were reduced, and different types of synthetic hormones were developed [16].
Today, the birth control pill is both a safe and effective birth control option.
Other short- and medium-acting methods
In addition to the pill, there are other methods that are so-called “short-acting”, which means the user needs to replenish them more often (think of the pill which is taken daily, compared to long-acting methods that can be in place for years at a time). Other methods are somewhere in between long- and short-acting, and these are helpfully called medium-acting methods.
The vaginal ring
In addition to the pill, the vaginal ring is another example of a short-acting method. It’s a small ring made of soft plastic that’s inserted into the vagina, where it releases hormones to prevent pregnancy. The very first vaginal ring, designed to be used for a month and then replaced, was FDA approved in 2001, adding one more birth control method to the market. In 2018, another type of vaginal ring which can be used for a full year was also FDA approved [17].
The birth control shot
There are also medium-acting methods, and one example is the birth control shot (also known as the depo shot or injection). It was FDA approved in 1992, but it actually became available in the rest of the world as early as 1971. Initially, there were concerns about whether the shot increased the risk of breast cancer, but studies concluded that this wasn’t the case, and the birth control shot is a safe and effective method that’s used by women globally to this day [3].
Long-acting reversible contraception (LARC)
The IUD: development, side effects, and FDA approval
The intrauterine device, or IUD, has drastically changed how we think about and use birth control. IUDs are highly effective (more than 99%), and paired with the convenience of using a long-term birth control method, make them a great option for lots of people.
The very first IUD was developed by Dr. Richard Richter, and this was made from silkworm gut (yes, you read that right). Even as developments of the IUD continued, silkworm continued to be used in the following decades as well. In the 1930s, silver wire was added, which made the device more effective at preventing pregnancy, but the silver also ended up being absorbed by the body and turning women’s gums blue and black [18]. Yikes. Silver IUDs went out of commission, but this did give an indication that metal can be effective in preventing pregnancy.
The evolution of IUDs continued, and the device we know today started taking form in the late 1960s, when Dr. Howard Tatum made a plastic, T-shaped IUD in an attempt to decrease side effects like cramps and bleeding. At the same time, studies on rabbits led to the discovery by Dr. Jaime Zipper that copper was effective in preventing pregnancy when placed inside the uterus. The two combined their discoveries, and the first copper IUD was created in 1969 [18].
However, it took a while still for the IUD to become widely available as birth control. A later version of the copper IUD was approved by the FDA in 1984, and it’s still in use today. The first hormonal IUD, on the other hand, wasn’t FDA approved until 2000 [18].
The implant
The research that led to the invention of the birth control implant dates back to the 1950s, when pellets containing progesterone were inserted under the skin of rabbits. It took a while for it to get to the human use stage, though. The first implant was approved by the World Health Organization (WHO) in 1984 to be used worldwide as a contraceptive, but the FDA lagged behind. It was only in 1990 that the implant was approved for use in the US [3].
Changing the game: Natural Cycles
While most advances in the history of birth control have been made within the field of medicine, the digital age has also paved the way for new innovations. In 2013, Swedish Physicist Elina Berglund was looking for a hormone-free way to prevent pregnancy. Not finding what she was looking for on the market, she decided to take things into her own hands — and so, Natural Cycles was created.
The NC° app builds on the science of the menstrual cycle and temperature tracking (similar to the fertility awareness methods we mentioned earlier). However, it takes it a step further by combining this knowledge with a customized algorithm that calculates your daily fertility status. By analyzing each user’s unique temperature data and cycle characteristics, along with optional ovulation tests, the NC° app provides natural birth control tailored to each individual.
At this point, you might be wondering, how does Natural Cycles compare to traditional fertility awareness methods? Great question. As it turns out, research shows that Natural Cycles finds fertile days more accurately than calendar-based methods since it adapts to each individual using their unique temperature and cycle data. Its effectiveness — 93% with typical use and 98% with perfect use — is also higher than other calendar-based methods as it relies on the science of body temperature [19].
Natural Cycles became CE marked in Europe in 2017, after a scientific study on more than 22,000 women confirmed the app’s effectiveness as birth control [20]. In 2018, Natural Cycles became FDA Cleared in the US as the first contraceptive app, making birth control history once again. To date, Natural Cycles is still the only available birth control app to be cleared by the FDA.
New innovations making NC° even easier to use
The NC° algorithm requires temperature data to provide a daily fertility status, and you can use a basal thermometer (which measures to two decimals) and input the data directly into the app, either by syncing via Bluetooth using the NC° Thermometer or manually. However, at Natural Cycles, we always continue to push for new innovations — including wearables.
In 2021, Natural Cycles received another FDA clearance, which allows the app to receive overnight temperature trend data from Oura Ring, making the measuring experience even smoother. This was followed by another clearance in 2023 by regulators in the U.S., Europe, and Australia, allowing the NC° app to use overnight wrist temperature data from Apple Watch. We’re constantly striving to offer more ways to measure, making NC° even more accessible for those who want to use it — watch this space for more wearable integrations!
Here, it’s also important to note that these wearables shouldn’t be used to prevent pregnancy on their own — the NC° app is still the only FDA Cleared and CE marked digital birth control.
Understand your options with Natural Cycles
Thanks for reading up on the fascinating history of birth control — it’s sure been a journey! Here at Natural Cycles, we believe that knowledge is power. Everyone should have access to information that enables them to make informed decisions about their own reproductive health, and that includes birth control. We know there’s no one size fits all when it comes to contraception — everyone has different needs, and our needs and wants even change throughout our lives. That’s why we’re proud to not only educate around different birth control options, but also offer a non-hormonal method in the form of NC° Birth Control — the first and only FDA Cleared and CE marked birth control app. Why not see if Natural Cycles could be right for you?
Did you enjoy reading this article?