Progesterone levels explained
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways
- Progesterone is a sex hormone that supports the reproductive system and plays a crucial role in the menstrual cycle and pregnancy
- Our progesterone levels vary throughout each menstrual cycle, and it is normal for levels to be higher during pregnancy and lower as we approach menopause
- Abnormally low or high progesterone levels can be a cause for concern, especially if you are pregnant or trying to conceive
Progesterone plays a vital role in the menstrual cycle, and our levels vary across cycle phases and throughout our lives. But what is progesterone, exactly? What does it do? And what are normal progesterone levels? Read on as we answer all of your questions about this hormone.
Progesterone plays a vital role in the menstrual cycle, and our levels vary across cycle phases and throughout our lives. But what is progesterone, exactly? What does it do? And what are normal progesterone levels? Read on as we answer all of your questions about this hormone.
What is progesterone?
Progesterone is a sex hormone found in both men and women [1]. It is one of the main hormones that support the female reproductive system, alongside estrogen, follicle-stimulating hormone, and luteinizing hormone. Progesterone is vital in the luteal phase of the menstrual cycle and early stages of pregnancy. In the female body, it is produced mainly by the corpus luteum and, during pregnancy, the placenta, with smaller amounts produced by the adrenal glands. [2].
Progesterone vs progestin
There is often confusion between progesterone and progestin. Progesterone is a naturally occurring hormone. Progestin, on the other hand, is a synthetic hormone that’s created in a lab and designed to mimic progesterone.
Progestins were initially developed primarily for hormonal contraception [3] and continue to be used in multiple forms of hormonal birth control, either in combination with estrogen or alone in progestin-only methods such as the mini-pill and implant.
Progestins prevent pregnancy by stopping the ovaries from releasing an egg each month and by thickening the cervical mucus, making it difficult for sperm to travel up the fallopian tubes and fertilize the egg [4]. Some forms of hormone therapy (also known as hormone replacement therapy or HRT) use progestins in treatment for perimenopause symptoms [5] and to protect the uterine lining from the effects of unopposed estrogen (when this hormone isn’t balanced by the presence of progesterone) [3].
Progesterone and the menstrual cycle
Let’s look at progesterone levels through the different phases of the menstrual cycle. Each cycle begins on the first day of your period, and this first phase is called the follicular phase. Your body is producing low levels of progesterone at this stage, averaging at 1mg per 24 hours [2].
After the follicular phase, ovulation happens when an egg cell is released, and a temporary gland forms from the empty egg follicle called the corpus luteum [2]. At this time and throughout the luteal phase, the corpus luteum produces progesterone, elevating your levels to up to around 25mg per 24 hours. This increase in progesterone prepares and stabilizes the uterine lining for potential implantation [2].
If the egg isn’t fertilized, and therefore implantation does not occur, the corpus luteum naturally breaks down. This lowers progesterone levels and causes the uterine lining to shed, which is the start of your period and your next cycle [2].
Progesterone and pregnancy
If the egg is fertilized and successfully implants into the uterine lining, pregnancy begins, and progesterone levels remain high. For the first eight to 12 weeks of pregnancy, the corpus luteum continues to provide progesterone. This hormone is crucial in the beginning for stimulating the uterine lining to deliver nutrients to the young embryo [6]. It also supports the function of the placenta, and between weeks eight and 12, the placenta takes over progesterone production and maintains the remainder of the pregnancy [6, 7].
Exact progesterone levels vary among individuals, but overall, as pregnancy progresses through the first, second, and third trimesters, progesterone levels gradually increase [8]. The higher progesterone levels throughout pregnancy prevent our bodies from releasing more eggs, signal to the uterus that it is not yet time for labour, and help prepare our breasts for breastfeeding [6].
Progesterone and miscarriage
Having some knowledge of hormonal shifts during pregnancy can be helpful when it comes to understanding the wider changes happening in your body. While small shifts in hormone levels should not be a cause for concern, there are some links between low progesterone levels and pregnancy loss [9]. If you are pregnant and have a history of three or more consecutive miscarriages, you may be offered progesterone, as some studies have shown potential benefit [10].
Progesterone and perimenopause
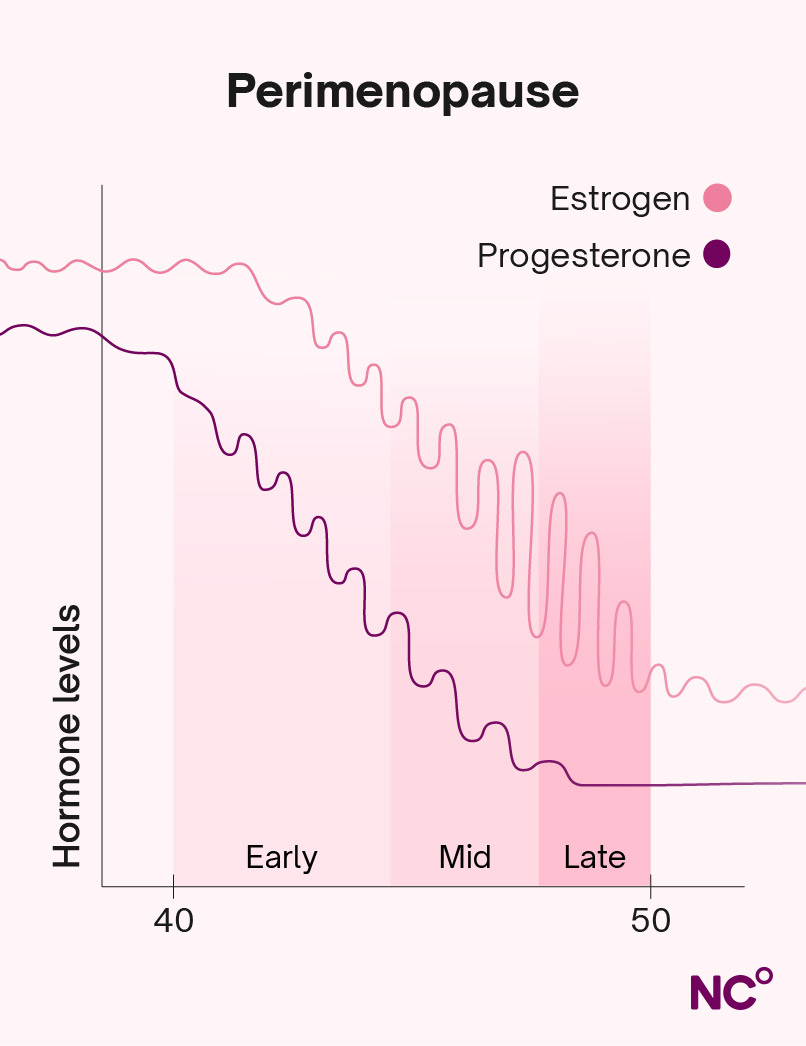
As we age, our hormone levels begin to fluctuate erratically, in preparation for the end of our periods (menopause). Perimenopause is the time before you reach menopause, when you may start to feel the onset of menopausal symptoms and often notice irregular periods. You officially reach menopause after you experience your final period, which is determined retrospectively 12 months after the fact [11].
During perimenopause, ovulation becomes less predictable. In some cycles, an egg is released; in others, there is no ovulation (referred to as anovulatory cycles). When you do ovulate, progesterone levels will rise, though often not as high or for as long as earlier in life. In anovulatory cycles, progesterone levels remain very low [12].
This drop in progesterone levels, coupled with erratic changes in estrogen levels, throws off the counterbalance between these two hormones that your body is used to. This imbalance is the culprit of the physical symptoms women experience during menopause, including night sweats, mood swings, and fatigue.
After menopause, you are no longer ovulating. Your adrenal glands will continue to produce some progesterone, but your levels will be much lower than before menopause [13]. The following illustrative chart shows the general pattern of progesterone decline during perimenopause.
Abnormal levels of progesterone
Low progesterone levels
Low progesterone is not only associated with perimenopause. Other conditions and physiological factors that can contribute to low progesterone include [14]:
- Ovulation problems - or experiencing anovulatory cycles.
- Polycystic ovary syndrome (PCOS) - This is a reproductive condition that causes irregular periods and often involves infrequent or absent ovulation, which means reduced corpus luteum formation and therefore lower progesterone exposure over time.
- High levels of stress - Chronic stress can disrupt hormonal signaling involved in ovulation, potentially leading to lower progesterone production.
- Luteal phase defect (LPD) - In this case, ovulation occurs, but the corpus luteum doesn’t produce enough progesterone or doesn’t last long enough to support the luteal phase [15].
If you are pregnant, low progesterone levels could be linked to:
- Pre-eclampsia - This is a complication occurring during or soon after pregnancy, characterized by high blood pressure [14].
- Ectopic pregnancy - This is a medical emergency, when a fertilized egg attaches itself to outside of the uterus, such as in the fallopian tube. Because the pregnancy cannot develop normally, progesterone levels are often lower [14].
- Miscarriage or pre-term labour - In early pregnancy, low progesterone levels are associated with pregnancy loss. Later in pregnancy, reduced progesterone activity can prompt the body to prepare for labour earlier than expected [16].
One of the most common symptoms of low progesterone is irregular or heavier periods. Other symptoms can be similar to those of perimenopause, such as hot flushes and trouble sleeping [14]. Having difficulty conceiving or experiencing fertility issues can also be a symptom of low progesterone [16]. A shorter luteal phase (10 days or less) is also associated with low progesterone [15].
Tracking your cycle with Natural Cycles can help you know when and if you ovulate, the length of your luteal phase, and spot patterns in your symptoms.
High progesterone levels
Just as you can have low progesterone levels, they can also be higher than average. High progesterone levels can cause symptoms such as bloating. Elevated levels aren’t usually anything to worry about, but could indicate underlying health conditions [14].
If you are concerned about abnormal levels of progesterone, it’s always a good idea to talk to your healthcare professional about your concerns and any symptoms you are experiencing.
Progesterone testing
There are several reasons your healthcare provider might want to test your progesterone levels, especially if you are pregnant or trying to conceive. These include [14]:
- To determine if you are ovulating
- Diagnosing or evaluating your risk of miscarriage or ectopic pregnancy
- In specific situations during a high-risk pregnancy
- To check the success of fertility treatments
- Find out the cause of abnormal bleeding
Get to know your cycle with Natural Cycles
Fluctuations in hormones and symptoms throughout our cycles are entirely normal, but can feel overwhelming. Natural Cycles is here to help. Whether you are looking to move to hormone-free birth control, are trying to conceive, or need support during pregnancy, after birth, or even during perimenopause, Natural Cycles empowers you to gain a deep understanding of each phase of your cycle. Our state-of-the-art algorithm uses body temperature and cycle data to pinpoint your fertile window, track your symptoms, and help you spot any patterns or changes from cycle to cycle.
Did you enjoy reading this article?