Late ovulation: Causes, symptoms & how to treat it
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways
- Everyone has their own unique cycle pattern, but ovulation can be considered to be late if it occurs later than usual for you, or if it results in the whole cycle being longer than 35 days
- Common causes of late ovulation include polycystic ovary syndrome (PCOS), stress, thyroid issues, hyperprolactinemia, and perimenopause
- You can notice a late ovulation if common ovulation signs happen later than usual for you — these include a positive LH test, or an increase in basal body temperature
Have you ever had a longer menstrual cycle than usual, or perhaps even skipped a period? Then it’s possible you may have had a late ovulation. However, if you’re not actively tracking your cycle, it might not be until your period is late that you notice something is different. Knowing when you ovulate is key when trying to get pregnant, but it can also help you understand your body and even prevent pregnancy if you’re looking for a hormone-free birth control option. In this article, we’ll dig into what late ovulation is and why it’s linked to longer cycles, plus we’ll cover some common causes, symptoms, and how you can help regulate your menstrual cycle.
What is late ovulation?
Ovulation, when an egg cell is released by one of the ovaries, typically happens around the mid-point of your cycle. While every cycle is unique and you won’t always ovulate on the same day in every cycle, ovulation is generally considered to be late if it happens later than your own usual pattern, leading to a longer cycle. Some people also consistently ovulate late and have longer cycles as a result.
We’ll dive deeper into the specifics of what late ovulation means in a minute, but first, let’s take a step back and look at some menstrual cycle basics.
What is a regular menstrual cycle?
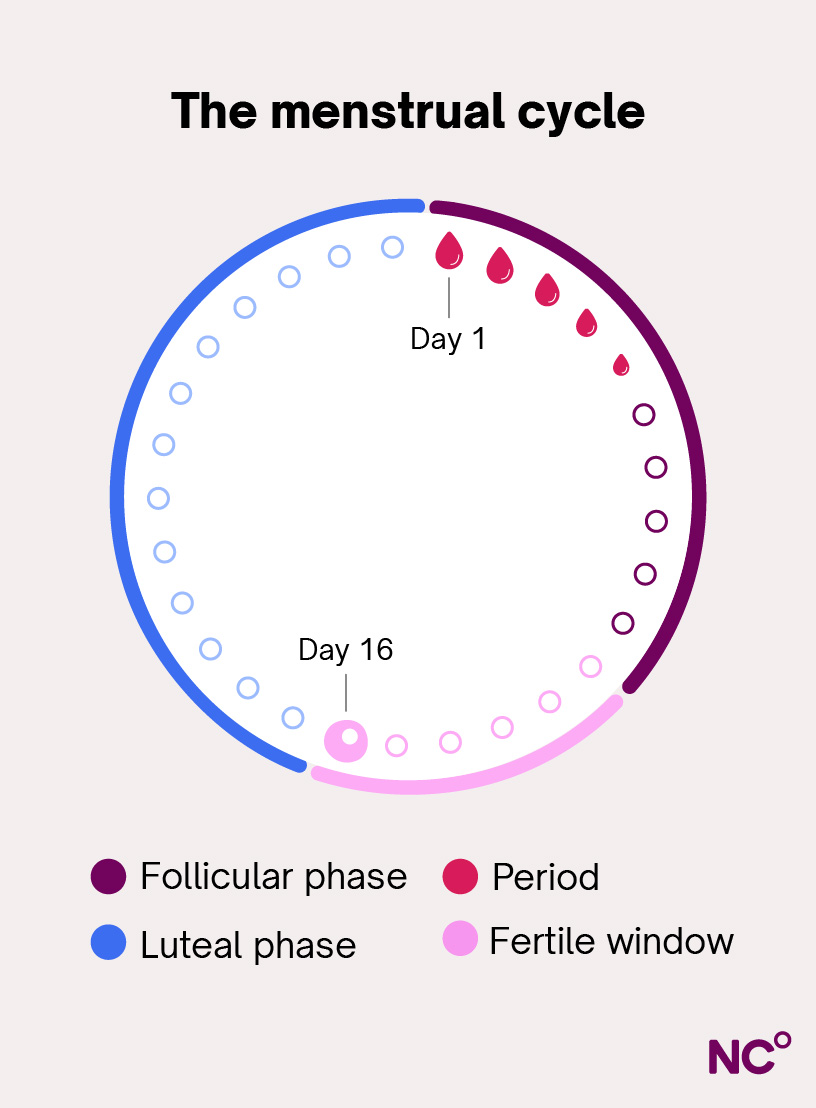
A new menstrual cycle begins on the first day of your period (this is cycle day one). Each cycle consists of two main phases, the follicular phase and the luteal phase, with ovulation marking the transition between them. Menstrual cycles naturally vary in length, both from person to person and from one cycle to another. However, cycles that are between 21 and 35 days long, and vary by less than 7 days from one cycle to the next, are generally considered regular [1].
The textbook menstrual cycle has long been believed to be 28 days long, with ovulation occurring right in the middle, on day 14. However, research done by Natural Cycles on over 600,000 cycles actually showed that the average length of Natural Cycles users was 29 days, with ovulation most often happening on day 18 [2].
Ovulation and cycle length — meaning when you can expect your next period — are closely linked. When two of your cycles differ in length, it’s usually because you’ve ovulated on different cycle days. This is due to the fact that the luteal phase (the second phase of the cycle) typically stays consistent in length in each of your cycles [2]. So, an early ovulation means a shorter cycle, while a later ovulation equals a longer cycle.
Understanding when ovulation is late
Now that we understand the pattern of the menstrual cycle, there are two ways we can define late ovulation.
- Late compared to your own individual ovulation pattern: For example, if you usually ovulate around day 16 of your cycle, and your ovulation suddenly happens on day 22, that would be a late ovulation for you. However, day 22 may be a normal ovulation day for someone else.
- Consistently late, resulting in cycles longer than 35 days: It’s also possible to ovulate regularly on a later cycle day — such as around day 28 — resulting in a consistent 42-day cycle. In such cases, ovulation may be perfectly predictable for that person, but the overall cycle length still falls outside the clinically defined “regular” range. These cycles are considered irregular and should be evaluated by a doctor.
In a lot of online fertility content, late ovulation is defined as ovulation happening after cycle day 21. However, healthcare professionals will generally use the definitions listed above and look at your individual menstrual cycle pattern when evaluating whether you ovulate late.
Does a late ovulation mean my period will be late?
Yes, if you ovulate later in your cycle, the whole cycle will most likely become longer. Once you ovulate, you can expect your period to start roughly two weeks later, as the luteal phase will most likely not change much [2]. In short, if your ovulation happens a week later than usual, that cycle will likely be around a week longer.
If you’re not tracking your ovulation, you may not notice that your ovulation was delayed until your period is late. Of course, your period can also be late if you’re pregnant — it’s often one of the earliest signs. However, if you know you’re not pregnant, it’s likely due to ovulation happening later than usual — something that can happen for a number of reasons.
What causes delayed ovulation?
There are many potential causes for a delayed ovulation, but before we dive in, it’s important to know that it’s normal for your cycles to change a little from one to the next. Even if your cycle is generally regular, ovulation won’t always occur on exactly the same day in each cycle. For example, in one cycle you might ovulate on cycle day 13 and in another on cycle day 15.
Additionally, a one-off late ovulation (for example, around a week later than usual) can happen to anyone, but there are also some conditions and circumstances that can delay ovulation or even cause anovulatory cycles (when ovulation doesn’t happen at all). Let’s take a look at a few!
Polycystic ovary syndrome (PCOS)
PCOS is one of the most common reasons for irregular cycles and affects as many as 6-13% of women of reproductive age worldwide [3]. Those with PCOS have higher levels of hormones called androgens (hormones that everyone has but are elevated in PCOS). They cause the follicles, which are the little sacs in the ovaries where the egg cells mature before ovulation, to have a harder time maturing and releasing an egg. As a result, ovulation may be delayed or not happen at all in some cycles [4].
Stress
Stress can affect our bodies in many different ways, including delaying ovulation. High stress levels or long-term stress can disrupt the balance of the hormones that govern the menstrual cycle and trigger ovulation. As a result, ovulation can be delayed or not happen at all in some cycles [5]. A certain amount of stress in our daily lives is normal, and it won’t always impact ovulation, but it’s still good to be aware of and keep an eye on how you’re feeling if you start to notice changes to your menstrual cycle during periods of high stress.
Thyroid issues
The thyroid gland is an organ that, among other functions, plays an important role in regulating our metabolism. It also produces thyroid hormones and is closely linked to the menstrual cycle. If your thyroid isn’t functioning as it should and the production of these hormones is disrupted, it can lead to irregularities like delayed ovulation or anovulatory cycles. Both hypothyroidism (an underactive thyroid) and hyperthyroidism (an overactive thyroid) can interfere with ovulation and cause irregular cycles. [6].
Giving birth and breastfeeding
After pregnancy, our bodies undergo hormonal shifts, and it can take several months for our ovulation and cycles to return. This process takes even longer for those who choose to breastfeed. While breastfeeding, our bodies produce higher levels of a hormone called prolactin, which triggers milk production. Prolactin also inhibits the hormones that are responsible for the development of egg cells in the ovaries and for triggering ovulation, which is most likely why ovulation can stop entirely or remain irregular while we breastfeed [7].
Because it suppresses ovulation, it is possible to use breastfeeding as birth control (also known as LAM or the lactational amenorrhea method) during the first few months after giving birth, as long as you’re breastfeeding exclusively [8]. However, there are a few conditions that must be met for this method to be effective, so make sure to consult with your healthcare provider if you’re curious about it.
Hyperprolactinemia
Hyperprolactinemia is a condition where the body produces too much prolactin, the hormone that naturally rises during breastfeeding. A common symptom of this condition is longer menstrual cycles — with late or missing ovulation — or in some cases, the menstrual cycle stops completely. Again, this is because prolactin suppresses the hormones that are involved in ovulation. This condition is treatable, usually with medications to lower prolactin levels [9].
Medications
Certain types of medications can affect the menstrual cycle and delay ovulation, including antipsychotics, some antidepressants, some blood pressure medications, and opioids [9]. It’s always best to check with your health care provider if you’re taking medications and have questions about your menstrual cycle or are trying to get pregnant.
There is also some research to suggest that so-called NSAIDs (Non-Steroidal Anti-Inflammatory Drugs), like meloxicam, ibuprofen, and naproxen, can delay or prevent ovulation from happening while they’re taken. However, the effect is likely temporary and goes away if treatment is stopped [10, 11, 12].
Perimenopause
In perimenopause, which is the transition leading up to menopause (your very last period), the menstrual cycle becomes increasingly irregular before it stops completely. Most of us enter perimenopause in our 40s or early 50s, usually between 45–55, and it can last for several years. In the first few years of perimenopause, it’s common to experience shorter cycles. Later on, cycles usually become longer with later ovulation than you may have had before (or skipping ovulation altogether). You may also notice other symptoms, like night sweats, joint pain, or brain fog [13].
Weight
Our weight is yet another factor that can impact our menstrual cycles and fertility. Both obesity and being underweight can disrupt our hormones and lead to more irregular menstrual cycles with late ovulation or anovulatory cycles (where no ovulation happens) [14, 15]. Additionally, weight gain is a common symptom in PCOS (which can cause late ovulation on its own), and it may make cycle irregularities more frequent [16].
Does late ovulation affect my chances of getting pregnant?
A late ovulation in itself will most often not affect your chances of getting pregnant. The fertile window — the six days in each menstrual cycle when it’s possible to become pregnant — consists of the five days leading up to ovulation and the ovulation day [17]. This means that if ovulation occurs later in a cycle, the entire fertile window shifts to occur later as well. And as long as you have sex during these fertile days, you have a chance of conceiving.
However, longer cycles mean that you’re not ovulating as often, and if your ovulation day changes a lot, it can be difficult to predict it. Having sex more frequently, or using Natural Cycles to learn your cycle patterns, could help if you’re trying to conceive..
Consistently late ovulations may also be an indication of other conditions, such as PCOS or thyroid issues, that may affect fertility, so it’s good to reach out to your healthcare provider if you regularly have cycles that are longer than 35 days.
Signs of late ovulation
There are several signs of ovulation you can keep track of during your cycle to understand when you ovulate. If you experience a late ovulation, these symptoms will naturally also be delayed compared to if you’d ovulated earlier.
- Cervical mucus changes: When we enter the fertile window and approach ovulation, our cervical mucus tends to become clear and stretchy, taking on an egg-white-like quality [18]. By keeping an eye on your cervical mucus during your cycle, you might notice these changes happening later in your cycle if ovulation is delayed.
- Later than usual LH surge: The level of luteinizing hormone (LH) usually starts increasing around one to two days before you ovulate and peaks a little less than a day before the egg is released. Though the exact timing of the LH rise will be individual, it will always happen before you ovulate, regardless of how late ovulation is [19]. If you use at-home urine ovulation tests, you may be able to catch your LH peak. But remember: a positive ovulation test isn’t a guarantee that ovulation has happened or will happen (even though it’s a good indication).
- Late temperature rise: Your basal body temperature (BBT) will increase by roughly 0.5–1°F (0.3–0.5°C) after ovulation and stay high until your period comes due to the rise in the hormone progesterone during the luteal phase [18]. By tracking your BBT throughout your cycle, you can spot if the temperature rise comes later than usual, indicating a late ovulation.
- Other ovulation symptoms are delayed: Of course, there are more symptoms that may pop up around ovulation, like ovulation pain, acne, or even bloating [20], so noticing the timing of those symptoms can also help you understand if your ovulation is late. However, it’s worth noting that these signs can be hard to interpret since they are individual and may occur in some cycles but not others, so they aren’t as reliable as temperature and LH test results.
- Longer cycle (late period): As we touched on earlier, a late ovulation will result in a longer cycle. So, if your period is late and you know you’re not pregnant, this can be a clue that your ovulation may have been delayed that cycle.
- The NC° app detects a late ovulation: If you’re using Natural Cycles, the app will detect your ovulation based on your body temperature and let you know which day it most likely happened — plus, it will predict your next period based on your ovulation date. The app lets you easily see if you’ve ovulated later than usual — so you’ll know if you can expect your period to also come later (remember: a late ovulation means a longer cycle). If you’re trying to get pregnant, you’ll know when to take a pregnancy test, and if you’re using the app as birth control, you’ll know why your period is late.
How to treat late ovulation
Ovulating later occasionally won’t likely require treatment — it can happen from time to time without there being anything “wrong”. However, if you have a medical condition that’s causing late ovulation or other symptoms, or if you’re struggling to conceive, there are ways to help trigger ovulation and regulate your cycle. Common treatments include ovulation-stimulating medications, medicines that help with insulin resistance, and hormone injections that support egg development [21, 22].
Treatment options will depend on why your ovulation is delayed, so it’s always a good idea to talk to your doctor if you’re concerned about your cycle — they’ll be able to help you find the right option for your situation. For example, if you have issues with your thyroid, the treatment would likely be thyroid hormone replacement and not specifically focused on ovulation.
When to see a doctor
Again, a one-off irregular cycle is normally nothing to worry about, but if it becomes a pattern, you should consult your healthcare provider. It’s also worth getting checked out if you notice your cycles suddenly become consistently different, for example, if they become much longer, or if you notice changes in bleeding patterns. You should always reach out if:
- You have irregular cycles (outside the range of 21–35 days, or that vary by more than 7 days from one cycle to the next) [1, 23]
- You haven’t had a period for three months, especially if it’s accompanied by symptoms like weight changes, fatigue, facial hair growth, or skin changes [1, 24]
- You have periods that last longer than 7 days or are very heavy [25]
- You’re tracking your ovulation and notice several anovulatory cycles, where ovulation doesn’t happen at all, even if the cycle length is regular
Can I treat late ovulation naturally?
As we mentioned, it all depends on why your ovulation is happening later. Some conditions require medical treatment, but there are also some lifestyle changes you can try to help support your body and menstrual cycle.
- Lower your stress levels: Since stress can have an impact on the menstrual cycle, reducing your stress levels can help improve things. We know it’s sometimes easier said than done, but try to make time for rest and get enough sleep. Mindfulness, meditation, or spending time in nature can also be helpful ways to lower stress levels.
- Nourish your body: To support your menstrual cycle, it’s important to eat a balanced diet with carbs, proteins, and healthy fats. Getting enough vitamins, as well as iron, could also have a positive effect on ovulation [15]. Consult your healthcare provider or dietitian if you have questions about changing your diet.
- Make time for movement: Regular exercise in a way you enjoy is a great way to promote general health and can help support your menstrual cycle. However, it’s also worth keeping in mind that excessive exercise can cause irregularities, especially if we don’t get enough energy from our food [15].
- Maintain a healthy weight: Maintaining a healthy weight can also help regulate the menstrual cycle [15]. However, just as with exercise, balance is key — we also need to eat enough for our menstrual cycle to function normally.
Healthy habits are important for our overall health as well as for our menstrual cycle, but it’s also important to keep in mind that sometimes, we need more support. Talk to your healthcare provider if you’re concerned about your cycle — they can help you find the best way forward.
Track your ovulation with Natural Cycles
Here at Natural Cycles, we believe that knowledge is power — and understanding when you ovulate can give you key insights into the rhythm of your body’s natural cycle. One of the core features of the NC° app is its ability to detect ovulation. By analyzing your body temperature throughout your cycles, measured with one of our integrated devices, the NC° Fertility Algorithm confirms your ovulation, identifies your fertile days, and predicts your next period — allowing you to prevent pregnancy naturally with NC° Birth Control, or pinpoint the days when you have the highest chance of conceiving with NC° Plan Pregnancy.
The app also helps you spot changes in your cycles and will notify you if something may require extra attention — plus, you can download your unique Cycle Report with your individual statistics to help you have productive conversations with your healthcare provider. Why not see if Natural Cycles could be right for you?
Did you enjoy reading this article?
