Non hormonal birth control methods: Effectiveness rates & how to choose
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways
- Non-hormonal birth control is a good option for those who want to avoid hormonal birth control methods (whether that’s due to side effects, risks, or any other reason)
- Non-hormonal methods include natural birth control, barrier methods, long-term birth control procedures, and more
- Consider factors like cost, side effects, protection against STIs, and future family plans when making your contraceptive choice with your healthcare professional
Are you considering your contraceptive options? If so, non-hormonal birth control is worth exploring. In this article, we’ve compiled a list of 11 non-hormonal contraception options, including natural birth control methods, to help you see all of your options in one place. You’ll find details about how each non-hormonal birth control works, their effectiveness, and the pros and cons so that you can have an informed conversation with your healthcare provider about what’s best for you.
Hormonal vs non-hormonal birth control
When it comes to choosing contraception, there’s no “one-size-fits-all” option. The birth control method that you decide on will depend on many factors and circumstances, like current lifestyle, future goals, relationship status, and more. These may change over time as well.
Some people opt for hormonal birth control if they’re looking for certain benefits like lighter periods, acne control, and less intense period cramps. But not everyone responds to hormonal birth control in this way, and there are some less desirable side effects of hormonal birth control as well, such as increased risk of blood clots and high blood pressure. Some types of hormonal contraception also may not work for you based on your habits and schedule. For example, if you don’t want to remember to take the pill every day, or if you need protection against sexually transmitted infections (STIs), hormonal birth control may not be suited to your lifestyle [1].
If you’d like to factor in these preferences and work with the natural hormonal cycle of your body, a non-hormonal birth control method might be a better option for you.
“Perfect” vs. “typical” birth control use
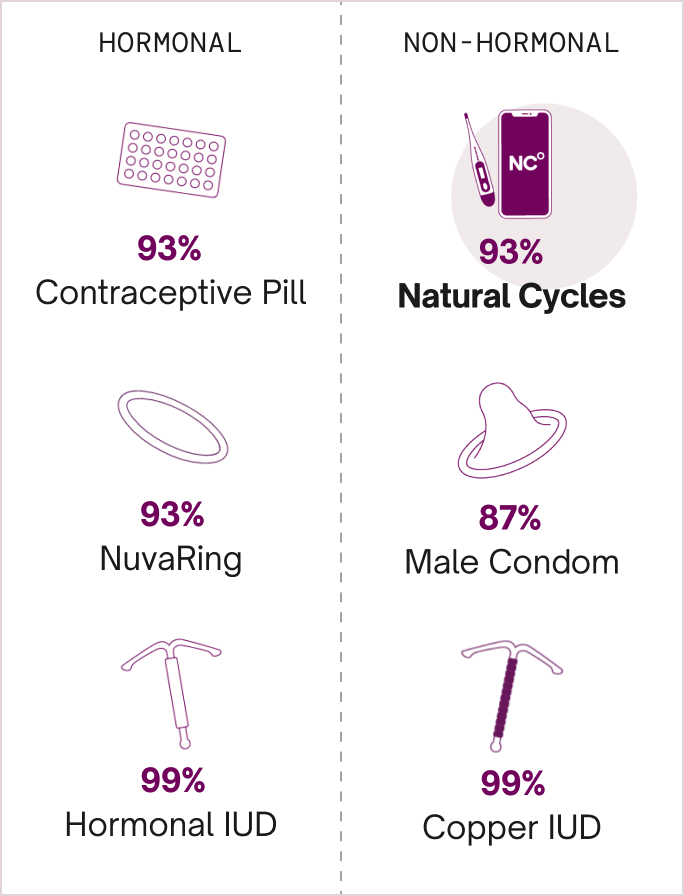
Before we dive into the details of the list, let’s go over one key difference to consider when looking at non-hormonal birth control: effectiveness with “perfect” and “typical” use. No birth control is 100% effective at preventing pregnancy (except abstinence), but some methods are more effective than others [2].
For example, the birth control pill is 93% effective at preventing pregnancy with typical use, and 99% effective with perfect use. “Typical use” reflects how the method is used in real life, e.g. forgetting to take the pill occasionally or taking it at the wrong time.. “Perfect use” means that the contraception is used as intended every single time. Back to our example, this means that 7 out of 100 women will experience an unintended pregnancy within one year of using the pill as contraception with typical use. This is an important factor to know while exploring your birth control choices [2].
Non-hormonal birth control options
Below, we’ve curated a list of 11 common non-hormonal birth control options and their uses and effectiveness, along with some pros and cons. We’ll start with natural birth control methods, move on to barrier birth control, explore long-term non-hormonal contraceptives, and end with a few alternative contraceptive methods. We hope this can help you have informed discussions with your healthcare professional..
Natural birth control methods
1. Natural Cycles
Natural Cycles is the first FDA Cleared birth control app in the United States. NC° Birth Control uses your basal body temperature, menstrual cycle data, and optional ovulation tests to predict your fertile window, similar to some fertility awareness methods (FAMs). You can choose to measure temperature with a basal thermometer or opt for one of our integrated wearables — Oura Ring or Apple Watch.
Unlike traditional FAMs and other tracking apps, Natural Cycles uses an algorithm that learns the pattern of your cycle and does the calculations for you. The algorithm will show you your daily fertility status in the form of either a “Red Day” or a “Green Day.” On green days, you’re not fertile and can have sex without protection. On red days, there’s a risk that you’re fertile and you’ll need to either use condoms or abstain from penetrative sex to prevent pregnancy. Since this method works with the natural processes of your body, it means that this birth control method is 100% hormone-free.
Natural Cycles is available online with an annual or monthly subscription. You can order it online or buy NC° Birth Control in select pharmacies.
Pros of Natural Cycles:
- Order online
- Non-invasive
- No side effects
- Less daily work than traditional FAMs
Cons of Natural Cycles:
- Doesn’t protect against STIs
- Must be 18+ to use
Perfect use: 98% effective [3]
Typical use: 93% effective [3]
2. Calendar methods
Calendar methods are a broad category that includes a range of natural family planning techniques, including Standard Days, the rhythm method, cervical mucus method, and body temperature measurement methods. All calendar methods rely on getting to know your fertility indicators, or by counting days to determine your own fertile window when you’re likely to conceive [4].
One of the main reasons people choose to use these methods is because they offer a natural way to prevent pregnancy. They don’t involve invasive procedures, using barrier methods, creams, or putting anything else in or on your body. However, they do require daily dedication and knowledge, and they require you to practice the method for at least three months before it can be relied on as natural birth control [4].
Pros of fertility awareness methods:
- No prescription needed
- Non-invasive
- No side effects
- Typically low or no cost
Cons of fertility awareness methods:
- 3-6 month monitoring period before it can be used for contraception
- Requires dedication and daily work
- Is subject to human error (e.g. counting cycle days incorrectly)
- Does not protect against STIs
Perfect use: 95% effective (Standard Days) [5]
Typical use: 88% effective (Standard Days) [5]
Barrier methods
3. Male condom
The most common type of condom is the male condom, also known as the external condom. It’s worn on the penis during sex and works to prevent pregnancy by collecting semen and acting as a barrier between the penis and the vagina. This stops sperm cells from meeting an egg cell, thus preventing conception and pregnancy. This method also helps stop the spread of certain STIs by preventing sexual skin-to-skin contact and swapping of fluids. Condoms can be used on their own or with another birth control method to add another layer of protection [6].
This male birth control option is pretty easy to obtain — you don’t need a prescription, and you can buy condoms in most supermarkets, drug stores, pharmacies, and more. Prefer not to leave the house to buy your contraception? No stress. You can also buy condoms online. If you have an allergic reaction to latex, it’s also possible to buy latex-free condoms [6].
Pros of male condom:
- No prescription needed
- Offers protection from STIs
- Affordable, easy to obtain and sometimes free in certain clinics
Cons of male condom:
- Needs to be used every time you have sex
- May take time and practice to learn how to use correctly
- Costs are involved
Perfect use: 98% effective [5]
Typical use: 87% effective [5]
4. Female condom
The female/internal condom, also known as the internal condom, is another barrier non-hormonal birth control method. It’s similar to the external condom in terms of how it works to prevent pregnancy and STIs, but it’s worn inside the vagina and also covers part of the vulva.
Some people prefer to use the internal condom as it puts the user in control. It’s important to note that an internal and external condom should not be worn at the same time during sex, as this increases the chances of friction and tearing [7].
Although you don’t need a prescription to access this method, female condoms are a bit harder to obtain. You can buy them online, or over the counter in some pharmacies. If you have a latex allergy, internal condoms are a good option because they’re latex-free, hypoallergenic, and made of nitrile (a soft plastic material) [7].
Pros of female condom:
- No prescription needed
- Protects against STIs
Cons of female condom:
- Needs to be used every time you have sex
- May take time and practice to learn how to use effectively
- Not as easy to buy as the male condom
- Costs are involved
Perfect use: 95% effective [5]
Typical use: 79% effective [5]
5. Contraceptive gels and creams
Non-hormonal contraceptive gels and creams work as chemical barriers to prevent pregnancy. There are two main kinds: spermicide and Phexxi. Both can be inserted into the vagina immediately or up to one hour before sex, but they work in slightly different ways. [8].
Spermicide contains a chemical that disables sperm so that they cannot swim, and also blocks the entrance to the cervix so that sperm cannot reach your fallopian tubes to fertilize the egg. Phexxi stops sperm from reaching the egg by lowering the pH in the vagina, creating an environment where sperm can’t move well or survive [8].
There are a few side effects of contraceptive gel, including vaginal burning and discomfort, increased chance of yeast infections, and bacterial vaginosis. Phexxi is also not recommended for those who are prone to urinary tract infections (UTIs). You can find spermicide at most drug stores and pharmacies over-the-counter, but you’ll need a prescription to use Phexxi. They also do not protect against STIs, notably [8].
Pros of contraceptive gel:
- Insert it up to an hour before sex
- Works with other types of contraception, such as a diaphragm
Cons of contraceptive gel:
- Prescription required (for Phexxi)
- Costs may be involved
- Some people may experience side effects
Perfect use: 84% effective (for spermicides) [5]
Typical use: 79% effective (for spermicides) [5]
6. Diaphragms and cervical caps
Diaphragms and cervical caps are also barrier birth control methods, but neither protects against STIs. They’re small objects made of silicone that sit inside the vagina and cover the cervix. This means that sperm cells cannot reach the egg cell during or after sex. For maximum effectiveness as birth control, they should be used with a spermicide [9, 10].
The main difference between the two is the shape — diaphragms are disc-shaped, while cervical caps look more like sailor hats. Another key difference is that diaphragms need to be left in place for at least six hours after sex, while cervical caps can be left inside the vagina for longer (up to two days after sex). Both of them can be inserted any time before sex [9, 10].
These non-hormonal birth control methods may not be right for you if you regularly get UTIs. You also need a prescription in order to buy them at a pharmacy, drugstore, or the like. For diaphragms specifically, a healthcare professional will need to fit you for one and show you how to use it before you can get started. Diaphragms and cervical caps are typically covered by insurance and are available for free in the UK on the NHS [9, 10].
Pros of diaphragms and cervical caps:
- Insert it any time before you have sex (more spermicide should be used if it’s more than three hours prior)
- You can use the same one for a year before it needs to be replaced
Cons of diaphragms and cervical caps:
- Requires fitting
- Requires a prescription
- Does not protect against STIs
Perfect use: 84% effective (for diaphragms) [5]
Typical use: 83% effective (for diaphragms) [5]
Long-term/permanent non-hormonal birth control methods
7. Copper intrauterine device (IUD)
If you’re looking for a long-term, non-hormonal contraception, the copper IUD might be a good fit for you. Also known as the copper coil, this t-shaped piece must be inserted by a healthcare professional and can sit in the uterus for up to ten years. It primarily prevents pregnancy by creating a hostile environment in the female reproductive tract, which inhibits sperm motility and survival and thus prevents fertilization. If used as emergency contraception within five days after unprotected sex, it can also prevent implantation [11].
The copper IUD is highly effective at preventing pregnancy. In fact, it’s more than 99% effective with both typical and perfect use. One of the reasons it’s so effective is that it requires little work from the user after it’s inserted — it can just sit there and effectively prevent pregnancy for years without you having to think about or maintain it. It doesn’t protect against STIs though, so if that’s a concern, you may still want to use condoms in conjunction with a copper IUD [12].
One of the great things about this method is that it can also be used as emergency contraception if fitted for up to five days after having unprotected sex. It’s also usually covered by insurance and available in the UK from the NHS. But some people who use this method of birth control may get unpleasant side effects such as longer or heavier periods, spotting between periods, or worse period pain. It’s also common to experience some pain or cramping during the fitting and in the following days [12].
Pros of copper IUD:
- Highly effective for years
- Doesn’t require any work once fitted
- Can be used as emergency contraception
Cons of copper IUD:
- Invasive
- Requires a professional to fit and remove
- Can have side effects, such as heavier or longer periods and pain
- Doesn’t protect against STIs
Perfect use: More than 99% effective [5]
Typical use: More than 99% effective [5]
8. Vasectomy (male sterilization)
Another long-term, non-hormonal birth control method is a vasectomy procedure. This is a surgery that involves cutting or sealing the tubes that carry sperm. It is intended to, and should be considered, permanent birth control, although it is possible to successfully reverse a vasectomy in some rare circumstances [13].
The procedure itself is quick, and although the individual may experience some mild discomfort, most people will be able to return to work after a day or two. After the procedure, you’ll need to use another method of contraception for several months to make sure there’s no residual sperm left. You’ll be asked to provide a sample after a few weeks to check that the procedure was successful. Physiologically, there are no changes to sex drive or hormone levels post-vasectomy, but it’s important to note that the procedure does not protect against STIs [13, 14].
Pros of vasectomy:
- Highly effective
- Long-term option
- Quick procedure with low down time
Cons of vasectomy:
- Permanent
- Invasive
- Costs can be involved depending on your country
- Does not protect against STIs
Perfect use: More than 99% effective [5]
Typical use: More than 99% effective [5]
9. Female sterilization (tubal ligation)
As with a vasectomy, female sterilization is more than 99% effective as a long-term non-hormonal birth control option. The procedure is called a tubal ligation and it works by permanently blocking or sealing the fallopian tubes. This surgery is a bit more complicated than male sterilization, and may require a general anesthetic and more recovery time [15].
Sterilization works right away, so it’s a “get-it-and-forget-it” birth control, but consult with your healthcare professional about when it’s safe to have sex again. It’s also worth noting that you’ll still get your period after having your tubes tied, and it also does not protect against STIs [15].
Pros of tubal ligation:
- Highly effective
- Long-term option
Cons of tubal ligation:
- Permanent
- Invasive
- Depending on country costs may be involved
- The procedure is not as quick and easy as with male sterilization and may require more recovery time
- Does not protect against STIs
Perfect use: More than 99% effective [5]
Typical use: More than99% effective [5]
Other methods
10. Pull out method
When it comes to preventing pregnancy, the pull out method (also known as the withdrawal method) has been around for a very long time. However, just because it’s tried and tested doesn’t mean it’s the best way to prevent pregnancy (far from it!). When it comes to failure rates, this method is only 80% effective with typical use. This means that 20 out of 100 people using the pull out method will get pregnant within a year [16].
The pull out method works by removing the penis from the vagina before ejaculation. This can be tricky to time, and even if it is done perfectly, there is still a risk of pregnancy. Sperm may present in pre-ejaculate, and there’s a risk of pregnancy if even only a small amount of sperm gets into the vagina. It also does not protect against STIs [16].
Pros of the pull-out method:
- Free
- Easily available
- Can be used with another form of contraception
Cons of the pull-out method:
- Hard to time
- Much less effective than other methods
- Does not protect against STIs
Perfect use: 96% effective [5]
Typical use: 80% effective [5]
11. Breastfeeding as birth control (lactational amenorrhea or LAM)
Lactational amenorrhea (or LAM for short) is another non-hormonal birth control method that is suitable for people who have just given birth and are breastfeeding full time This means you’re only feeding your baby breast milk directly (no pumping), and the gaps between feeds are no longer than four hours during the day and six hours at night [17]. During this time, your body naturally stops ovulating. When ovulation stops, you’re not fertile and cannot get pregnant. You can use breastfeeding as contraception for up to six months, or until your period naturally returns.
Keep in mind that this is only a temporary option, and you’ll need to find another birth control method after six months or as soon as your period has returned. Due to the way the menstrual cycle works, you’ll ovulate before you get your first period after pregnancy again, which means that you may be fertile before you know you are. It’s important to follow the guidelines of LAM to use it effectively [17].
Pros of breastfeeding as birth control:
- Free
- Convenient if you’re already planning to breastfeed full time
Cons of breastfeeding as birth control:
- Requires daily dedication
- Only works for a short period of time
- Does not protect against STIs
Perfect use: More than 99% effective (during the first six months after delivery) [18]
Typical use: 98% effective [18]
How to choose a non-hormonal birth control option
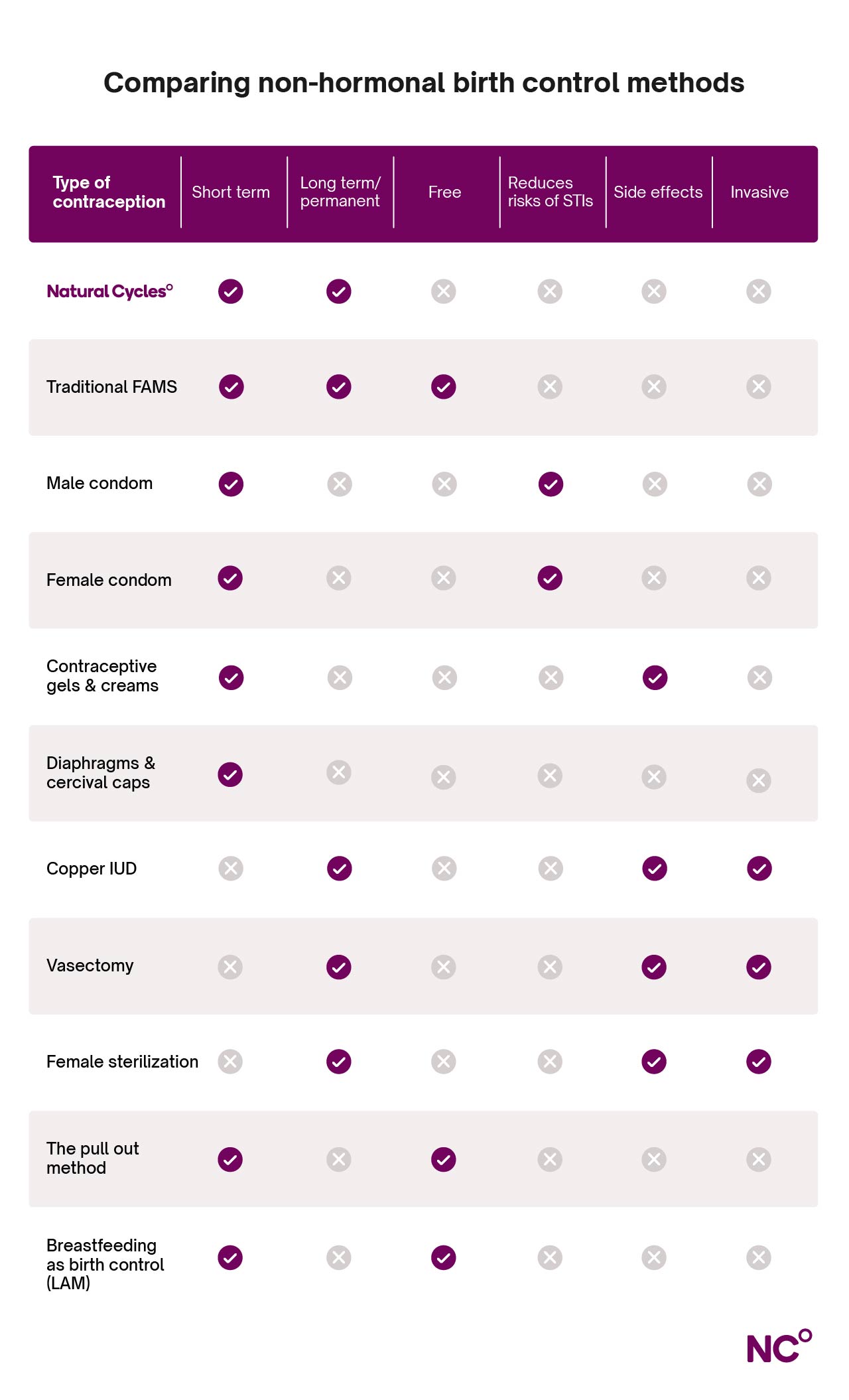
With all of that information about the non-hormonal birth control options available to you, you may be wondering how to make the right choice that will fit your unique needs. Some questions you may want to consider when choosing a non-hormonal birth control include:
- Do I want a permanent or short-term solution?
- What side effects can I handle? Which ones do I want to avoid?
- Am I comfortable with an invasive procedure?
- Do I need protection against STIs?
- How much does it cost?
Answering these questions for yourself can help narrow down the list above before speaking with your healthcare provider about your choice [19]. Here’s a handy table to use for reference with some of the most common considerations:
Ready to go hormone-free?
Thanks for checking out our roundup of non-hormonal birth control. We hope you’ve learned a bit more non-hormonal birth control and the options available to you. If you’re thinking about switching contraception methods, it’s always a good idea to talk to your reproductive healthcare professional about your options. They’ll be able to provide counseling and patient education to help you make an informed choice.
Natural Cycles is the first FDA Cleared birth control app, putting the power of your cycle in your hands. Hormone-free and non-invasive, find out if Natural Cycles could work for you today.
Did you enjoy reading this article?